
‘Whatever you do don’t get into this. There’s nothing you can do. It will only send you mad.’
Sage words from a gastroenterologist I’d never met before. A patient of his had a ruptured bowel – the pressure of gas, delivered during colonoscopy, far too high. He’d tried for years to introduce a safety mechanism to limit gas pressure. He’d failed.
We were sat at the back of an auditorium listening to Dr Terry Fairbanks – I absorbed everything he said.
So what was the gastroenterologist trying to save me from?
The prospect of helping save hundreds of thousands of lives in a system which doesn’t allow it. A sure pathway to madness.
Welcome to healthcare safety…..
Then I discovered my hat. I wear it proudly now – many colleagues curious as to why.
Some nurses comment – ‘It’s a great idea, we should all wear hats like this’ – to which I reply ‘You can’.
But they can’t – it hasn’t come via the ‘proper’ channels. We’re conditioned in a hierarchical top down system – step outside this at your peril – it’s far more likely to end your career than deliver change. I know – I’ve touched that void.
One group started wearing the hats only for a nurse in charge to insist they stop. They were told it looked ‘unprofessional’ – perhaps what was really meant was ‘non-conformist’. It doesn’t matter – they got the message.
Wearing a cotton hat with a name & role on may lead to a ban on cotton hats – infection control used to stifle an initiative that hasn’t come from the top. However there’s no evidence cotton hats lead to increased infection rates.
Knowing names & roles, great for camaraderie, is a skill essential for optimal teamwork. The World Health Organisation have numerous adverse event reports from staff misidentification. Unfortunately we can’t access these stories – error reporting systems lack transparency and don’t intercommunicate.
I’ve heard of medical students mistaken for senior trainees then instructed to finish operations. Arrests where requests to perform cardiac compressions aren’t followed for some time – no one knowing who the request was directed at.
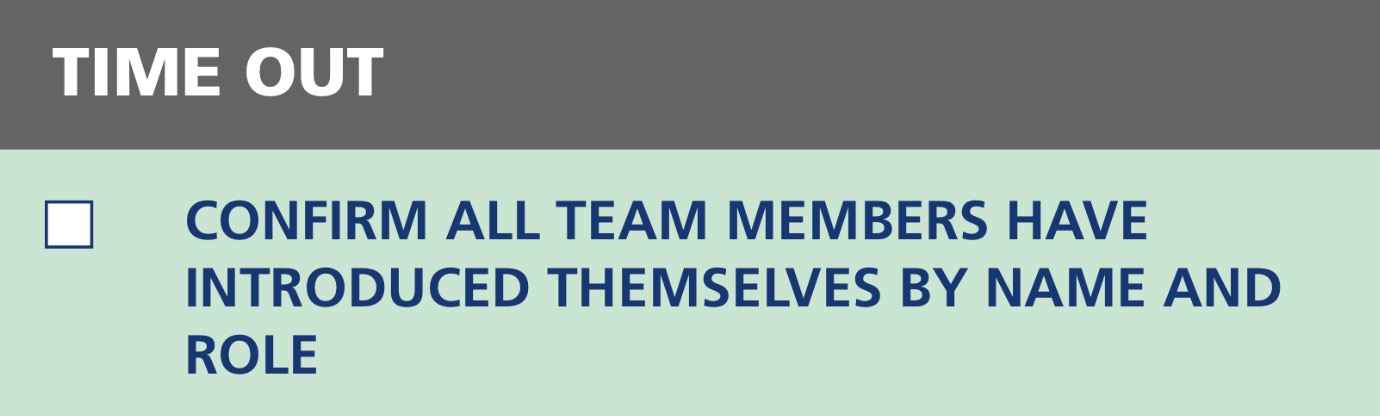
The WHO introduced a tick box to ensure theatre staff introduce themselves prior to every operation.
This box is always ticked yet the procedure rarely performed. Without access to the stories of adversity it’s just another tick box.
Even at the highest levels in healthcare the best ways to deliver safety are poorly known. We simply haven’t learnt the human factors approach. Dr Fairbanks knows – he’s a system safety expert who then went to work in healthcare – he describes this career path as ‘the quickest way to become psychotic‘.
I support the team ‘name & role’ tick box, yet there’s another more effective way to complement this taking into account human factors (we don’t always remember names after first introduction) and the complexity of our work environments (e.g. those who rush to help with a cardiac arrest weren’t in the room during the introductions).
Understanding why we aren’t already wearing named hats requires understanding how we’re deeply conditioned in healthcare.
We search for reasons to maintain the status quo – in changing we have to accept we weren’t doing things well enough.
A colleague stated he couldn’t envisage a single instance in his 30 years where displaying his name and role would’ve improved patient outcomes. There’s so many obstacles to patient safety – perhaps the first is accepting there’s a problem.
Some staff ask quizzically – ‘Can’t you remember your name?’. I’ve learnt not to say ‘If I couldn’t remember my name I’d write it somewhere I could actually see it’.
Others have said ‘I’d do the same but I don’t want to look stupid’ – while wearing what is essentially a pair of pyjamas – theatre scrubs.
Perhaps it reveals something we don’t like to admit – we’re all human and all make mistakes – we forget one another’s names.
If we struggle to adopt such a simple effective intervention just consider all the others we’ve stifled. These effective interventions were exactly what Dr Fairbanks was talking about.
He picked a handful of unnecessary front line hazards describing how each one repeatedly causes patients to suffer. I was enlightened – those things which had frustrated me for years, badly designed processes and equipment – they’re killing our patients.
Sadly the gastroenterologist knew, as things stand in healthcare, there’s nothing we can do about it.
He knew about the command and control structures. He knew the impact of competition and egos and how evidence and cost are used as tools to prevent change. He knew bystanders wise enough not to rock the boat. He knew that error reporting systems lack transparency making dispersed adverse events appear extremely rare – they’re not – the same adverse events happen again and again. He knew about bad apple theory and the focus on blame. He knew about the unchecked complexity of front line environments and that interventions delivered from the top have little effect. He was suspicious of greed and corruption at the highest levels preventing improvement.
He knew I’d learn this all myself. He could see it in my eyes. And he knew I’d push all the way and be faced with the most blunt instruments of all – bullying, threats and intimidation – called into a room and informed by a superior ‘I don’t care who you are or what you do but if you do anything like this again you are out.’
(Thanks for that – healthcare showing it’s true colours)
Perhaps what the he didn’t realize when warning me of my impending fate was that I was already too far gone – perhaps as mad as a hatter.
My hat’s a hands-free patient safety agitation device.
I won’t deny it’s difficult working in a system so averse to change while patients die and colleagues suffer unnecessarily every day. I’m constantly learning, improving and assessing the best way forward. Eventually something has to give and I won’t let it be me – it will have to be the even madder system I work within.
Solutions need to be driven not from the top but from the front line aided by system safety experts like Dr Fairbanks and facilitated by those in charge.
We need frameworks to deliver this – so here’s one – please check it out & help in any way you can.
It may well save your life.

Medical error has been reported as the third greatest cause of death. We shouldn’t expect this to change if we aren’t prepared to change ourselves. Change can be simple yet requires a lot of courage. For those brave enough for the #TheatreCapChallenge we salute you:


32 Comments