Having discussed coronavirus management with Chinese colleagues and reviewed numerous sources of information it’s a burning question:
Are the Personal Protective Equipment policies in Australia inadequate?
Hospitals are a major transmission area for coronavirus
Coronavirus is highly transmissible – it’s present in our breath, hangs around in still air for up to 4 hours and can last on surfaces for 3 or 4 days.
Many people transmitting coronavirus may be completely unaware they have it – being asymptomatic or pre-symptomatic.
A major take-home message from Mrs Hu – senior ICU nurse in Wuhan – was the risk of staff to staff transmission of coronavirus. Mrs Hu particularly wanted to emphasise this – it is seen as a much greater issue than patient to staff transmission.
One specific way to help combat this is for all staff and patients within hospitals to wear masks at all times – this is the policy in Wuhan.
This can be contrasted with Australian Health policy guidelines which indicate masks only need to be worn during patient interaction.
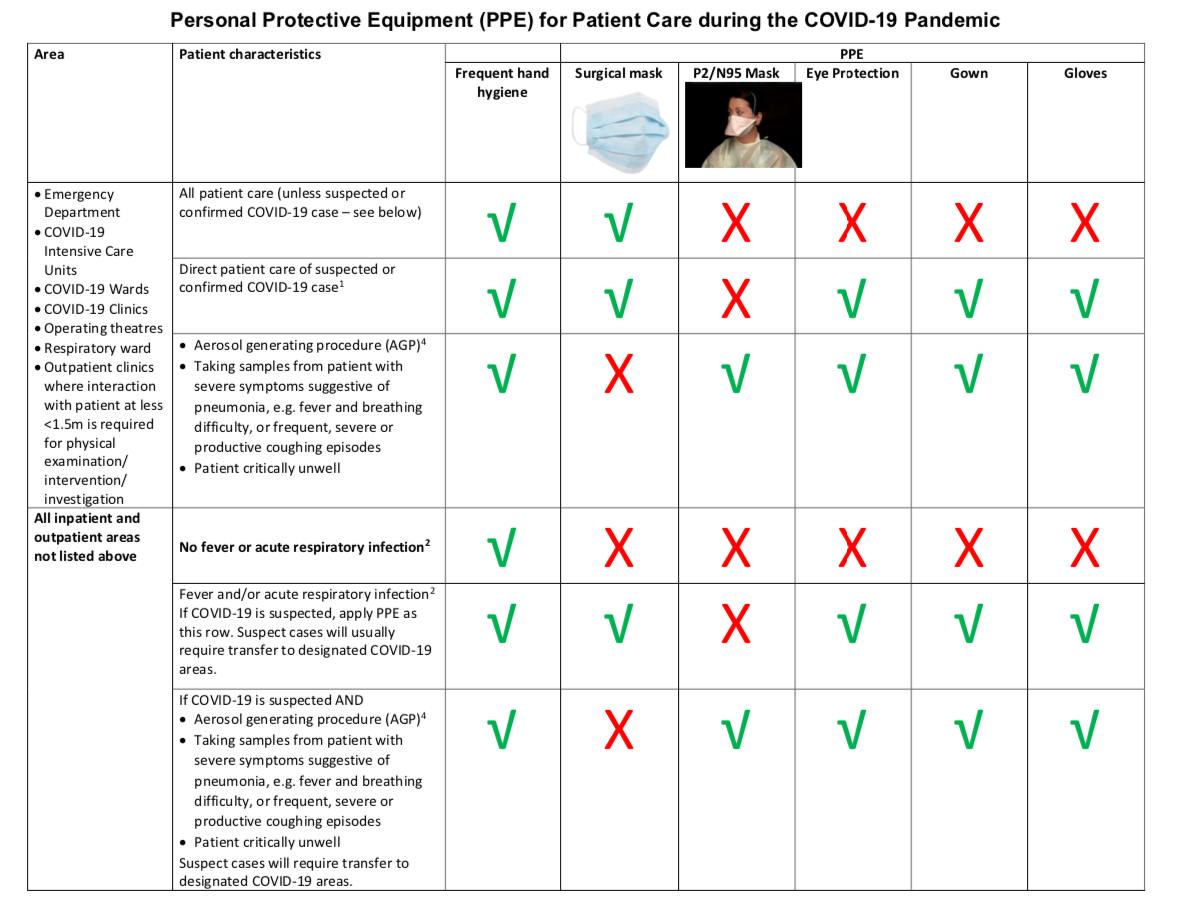
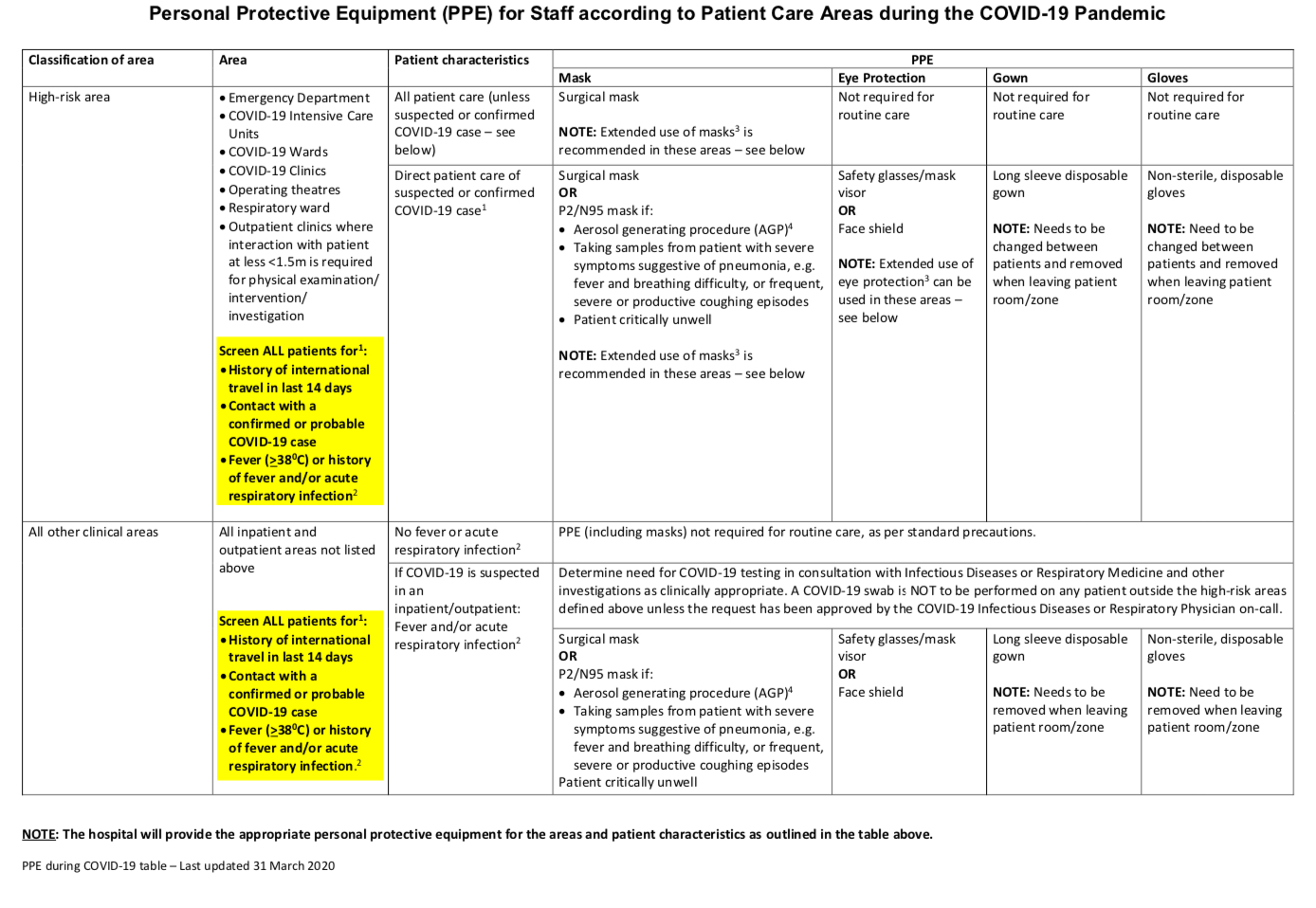
Patient Care Areas
Another profound issue relates to the level of testing we perform and how this impacts on designating different areas for coronavirus management within hospitals.
Within Australia we’ve only divided our hospitals into 2 Patient Care Areas
- High risk areas
- All other clinical areas
Within China areas are divided into 3 distinct zones. It is noted that these zones should ideally be in completely seperate buildings where possible.
- COVID positive
- COVID suspected
- COVID negative
Achieving a COVID negative diagnosis is very stringent and requires being asymptomatic, not having been in contact with known coronavirus patients and having 2 tests 24hours apart where coronavirus is not detected.
(It’s important people are aware that a ‘coronavirus not detected’ test result does not mean one is negative for coronavirus – there are many reasons for false negatives).
Testing
All staff within Wuhan’s hospitals are tested on a regular basis. Those caring for known coronavirus patients are not allowed home after their shifts but live in designated hotels and also isolated. They need to isolate for 14 days prior to returning home. Mrs Hu did not return home for 2 months given the amount of time she cared for coronavirus positive patients in her ICU.
Because our testing does not reach the same stringent standards it would be best to consider that all staff and patients currently in our operating hospitals may be suspected of having coronavirus.
It may be pertinent to create Coronavirus negative hospitals, which have been cleared and disinfected prior to use, to care for those deemed coronavirus negative using the same stringent criteria as those in China.
Personal Protective Equipment
Not only do we not have enough PPE, the PPE that we do have, particularly the gowns we are using, appear to be the wrong type.
Hooded Gowns
The gowns we are using in Australia do not provide head and neck covering and leave many areas of face, head and neck exposed.
Goggles
The goggles we should use need to provide a close to air tight seal.
Often within Australia staff are not wearing goggles or are simply wearing protective glasses.
Masks
Within Wuhan, where surgical masks are used, 2 surgical masks are used over one another for up to 4 hours.
N95 – N95 masks can be used for up to 8 hours. It is important that these are fit tested – the wearer applying them to their face and performing a suction test. It is ideal that hospitals have a number of different sizes and types of N95 masks to accommodate for the many different face shapes
Tape
The whole set up – hooded gown, N95 mask, goggles is also fit suction tested. If the set up does not suck down onto the face then tape is applied around those areas where air is getting in to make an air tight seal.

Double gloves and boot covers are also utilised.
Inadequate PPE
With inadequate PPE staff are unnecessarily transmitting coronavirus to one another.
There’s an increasing noise from the front line yet the voices of front line staff are often being silenced through threats from hospital administrators.
Having spoken with psychiatry colleagues the worst levels of Post Traumatic Stress Disorder occur through being disempowered and threatened when trying to do the right thing.
Will front line staff who do not succumb to coronavirus succumb from the resultant PTSD?
If you can help please do.
We are desperately sourcing Personal Protective Equipment from across the world to protect front line staff, patients, the community and the future integrity of healthcare.
Please Help.


One Comment