Perhaps ergonomics is about designing the environment, of which we are an inextricable part, in order to achieve desired outcomes.
Improved patient care definitely to be desired.
I put this to a great mentor of mine – he illustrated how it would never be that easy – like expecting atheists upon reading the bible to suddenly believe in god.
I was sunk.
Yet my mentor suggested I read the works of Dr Ronald Heifetz on ‘adaptive change’ – I’d never come across the term.
Dr Heifetz spends the first 3 chapters of his book pleading with the reader to go away, forget about it, have a normal life. He explains that trying to deliver change, which requires constant agitation, would only lead to a lifetime of frustration and trouble.
However perhaps for some the alternative is worse.
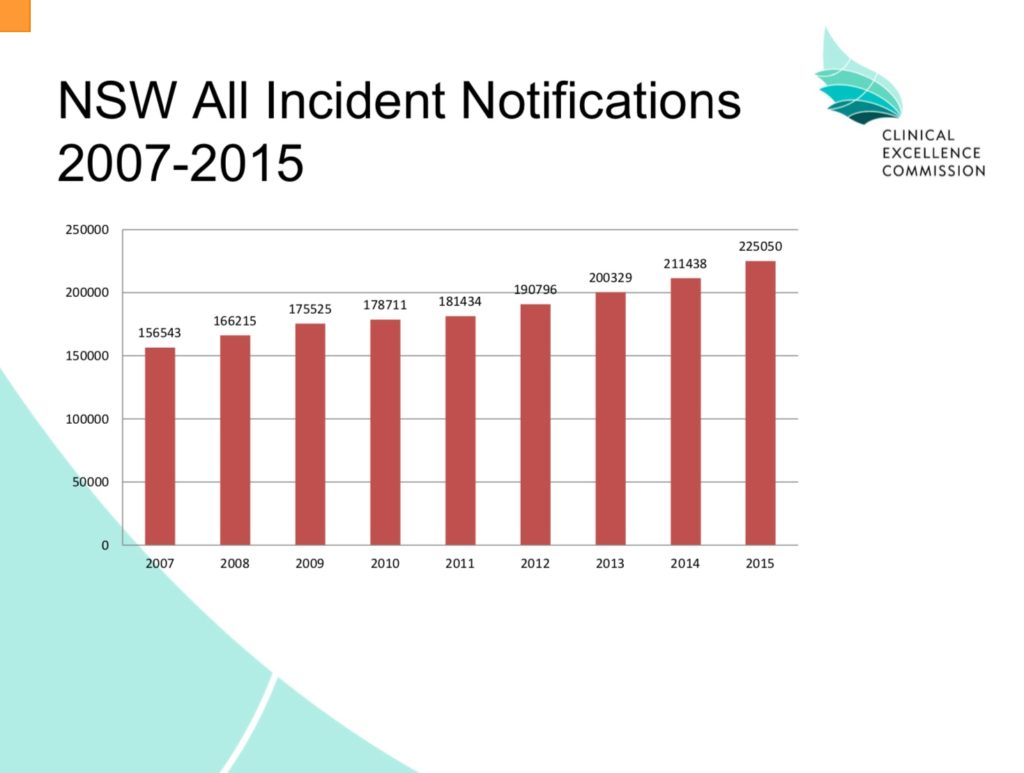
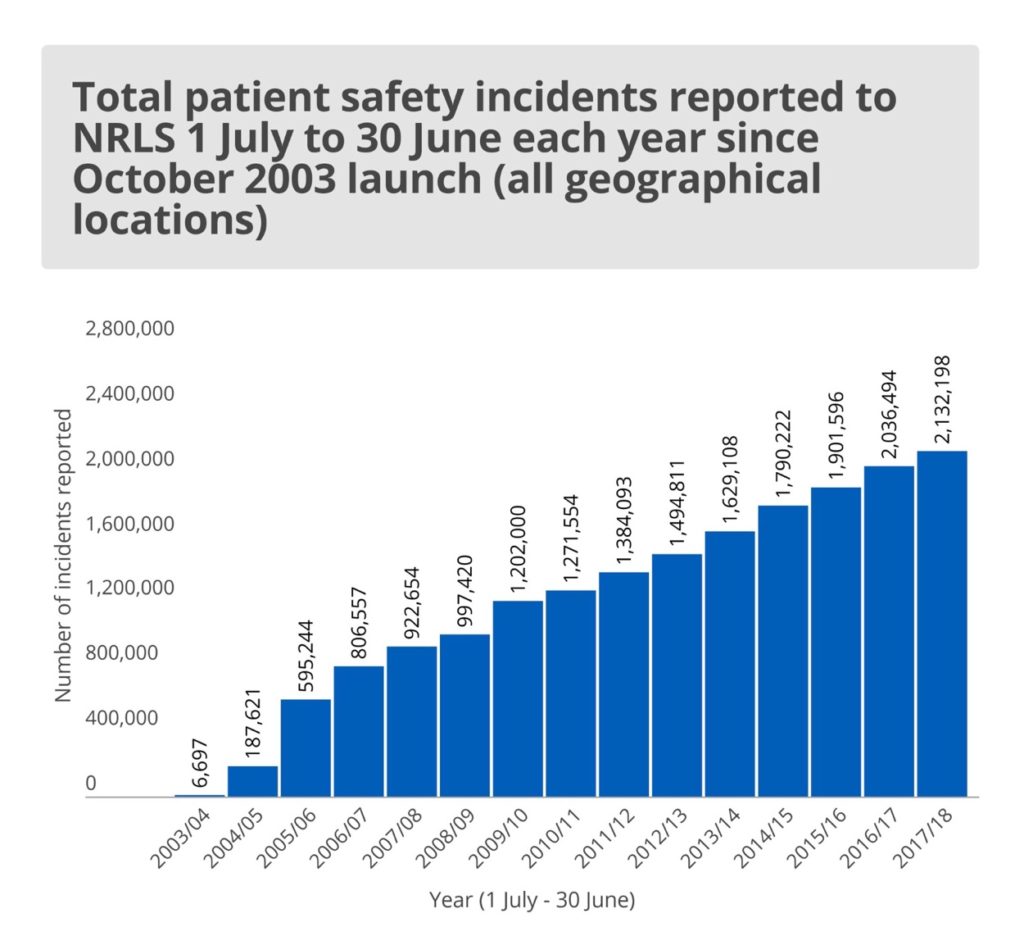
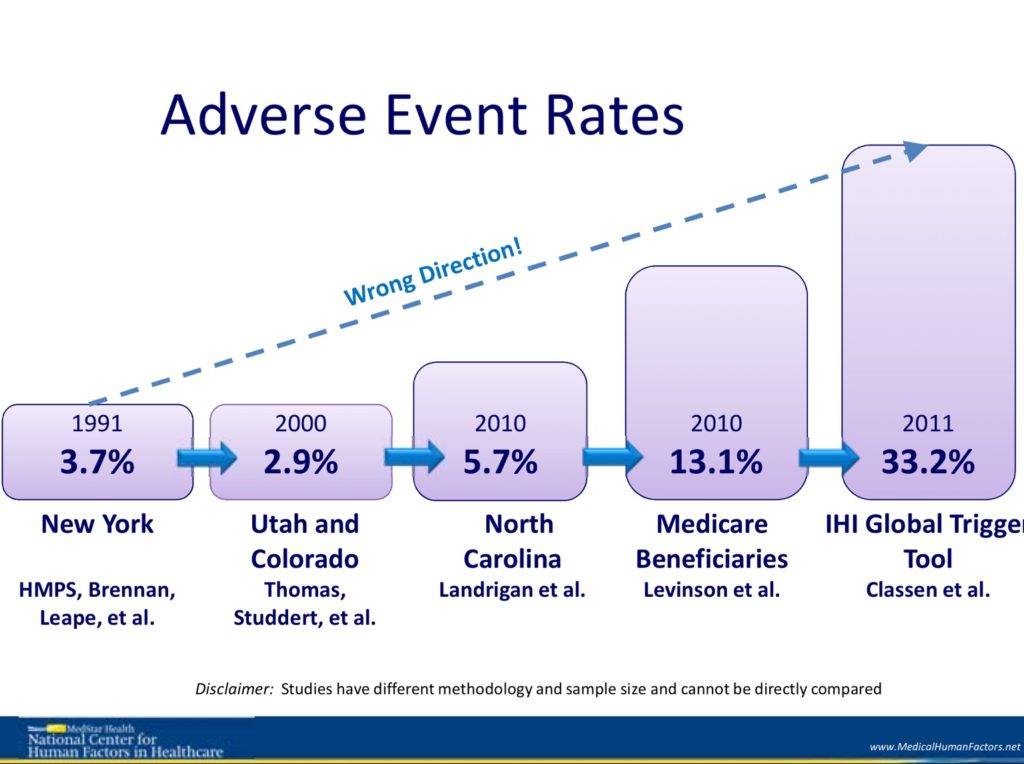
How can one do nothing when the medical error issue is so bad and only appears to be increasing.
How can we not try when realising every day things will only become worse.
I mean I chose to work in a profession dedicated to protecting the life and wellbeing of others?
Didn’t I?
Didn’t we all?
I’ve still to meet a single healthcare staff member who doesn’t want the best for every patient.
Isn’t that enough?
Why are we still heading in the wrong direction?
Since attending the Terry Fairbanks presentations I’ve become increasingly aware of the unnecessary hazards, dreadfully designed systems and equipment which contribute to immeasurable patient harm. There are tonnes. At the same time I’ve become increasingly aware of our inability to remove them.
Front line staff completely disempowered, numb even, so much so that often we can’t see the hazards any more – what’s the point – suggesting change most likely to lead to a world of pain, careers threatened.
So shut up.
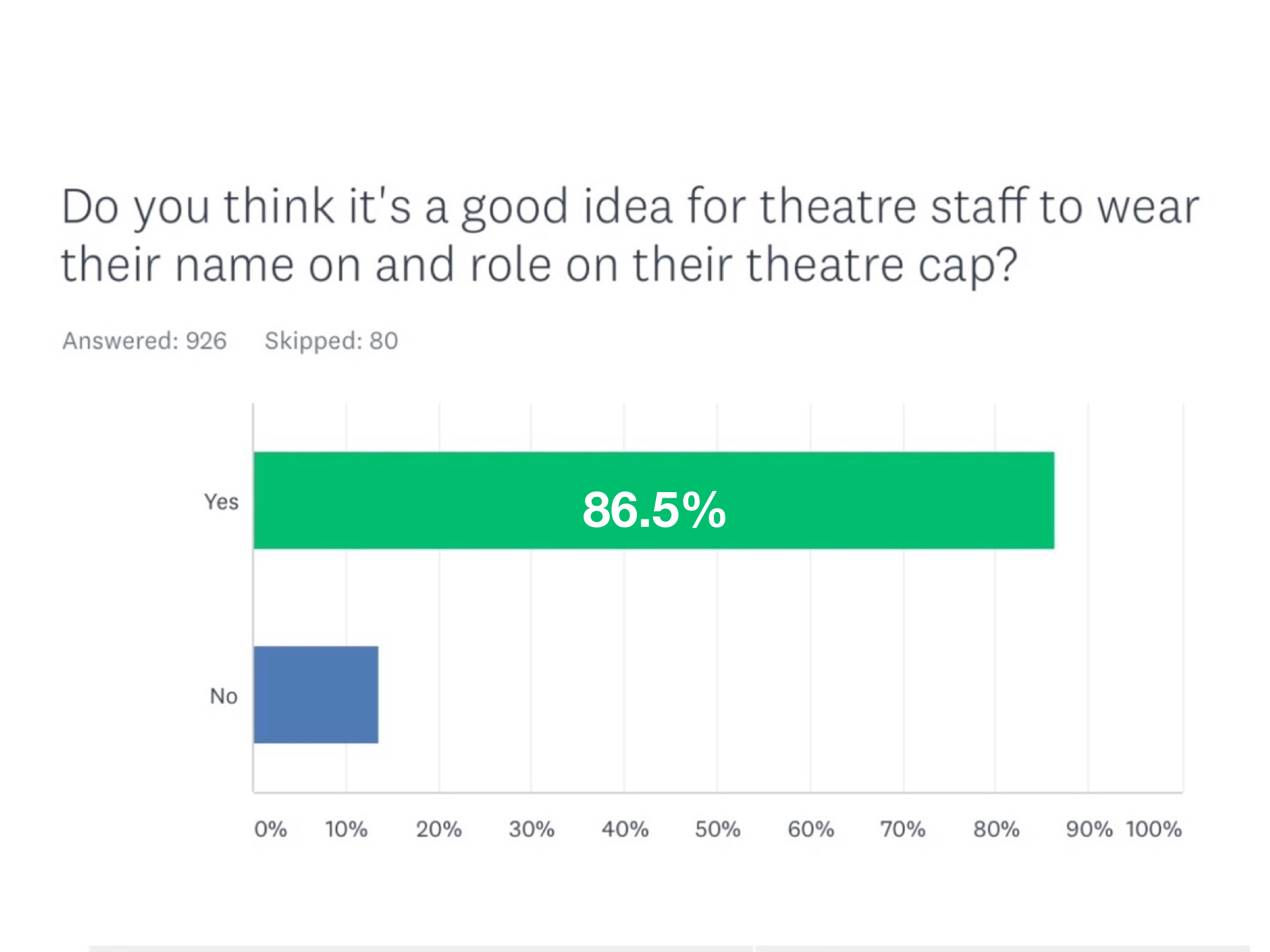
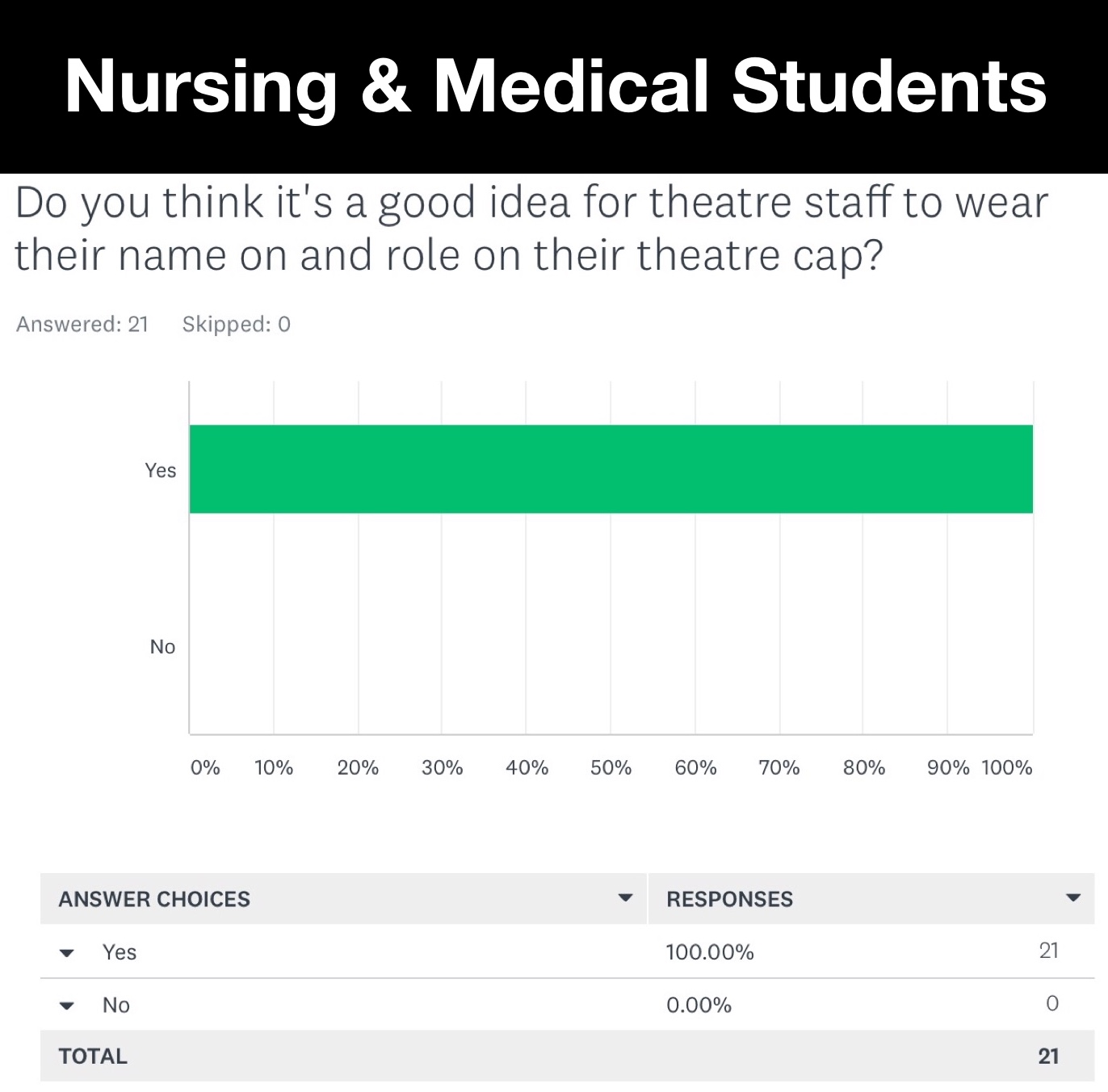
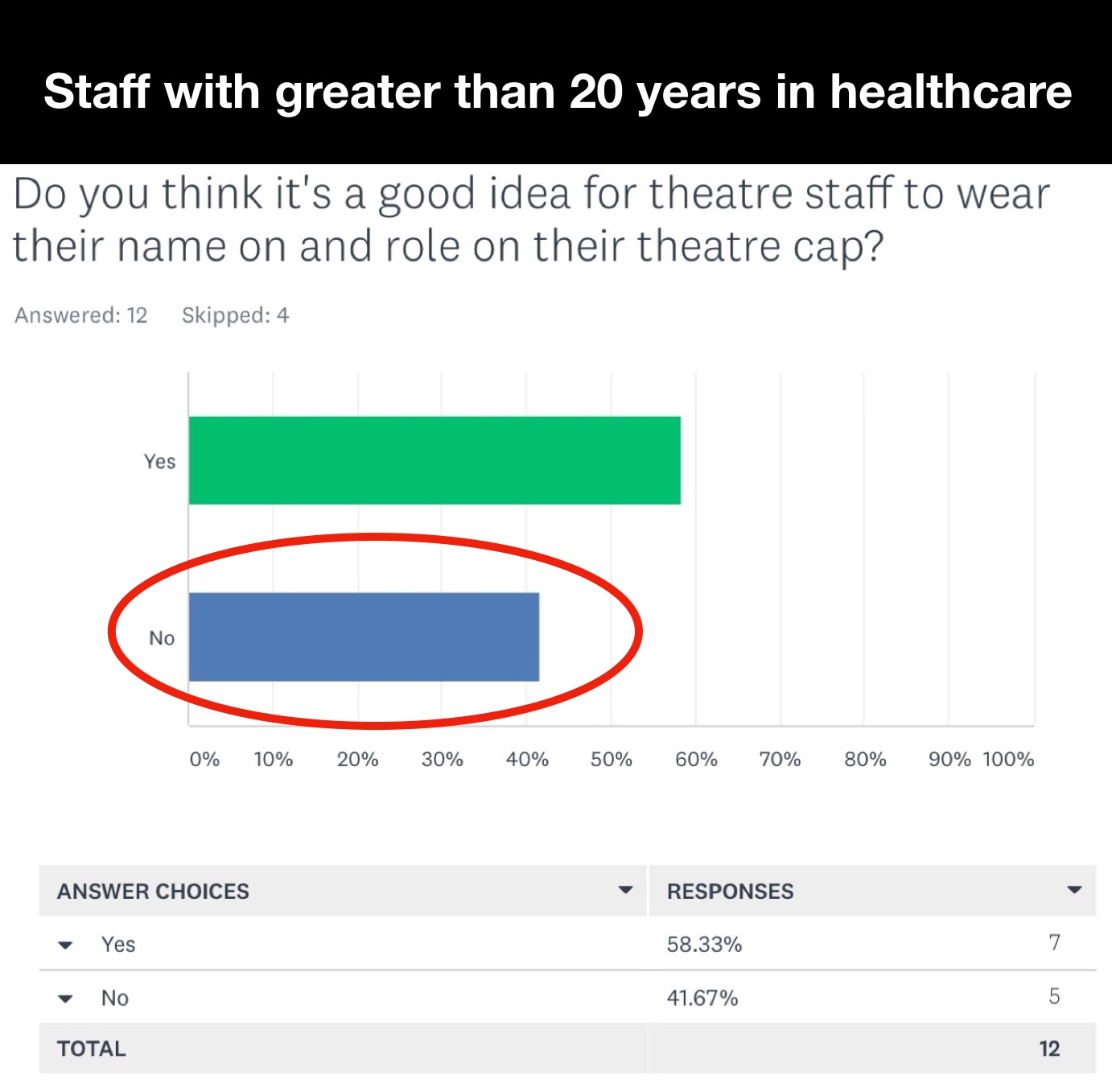
Perhaps Alison Brindle however gave us an ‘in’ with her #TheatreCapChallenge. This patient safety improvement is obvious (to most) yet at times it’s been vehemently resisted – an opportunity to explore the healthcare problem and display it to the world.
For in understanding it perhaps then we can fix it.
So here goes….
Healthcare is a highly emotive fear driven industry.
Our top down structures support conformity and nurture the most competitive conformists into positions of power.
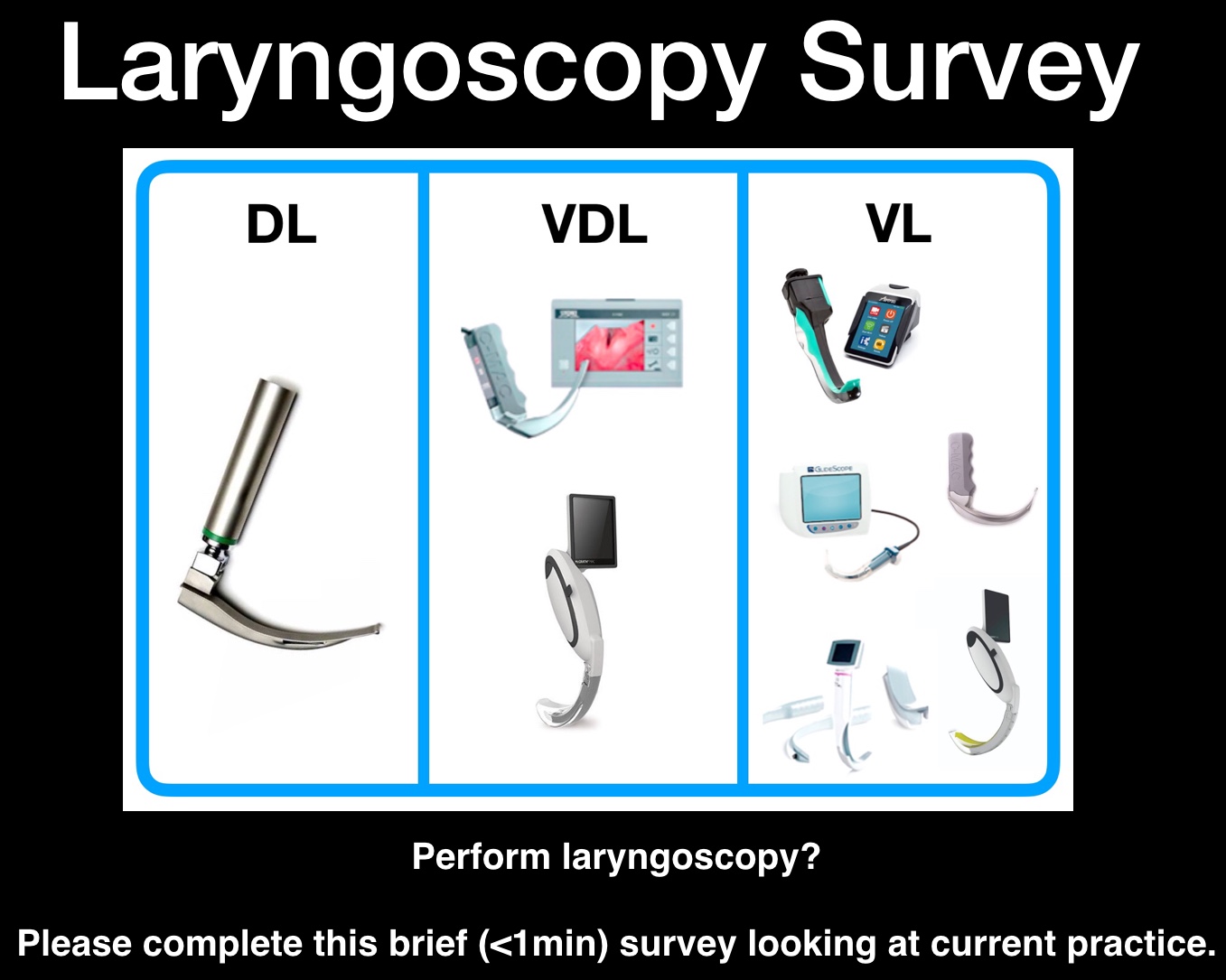
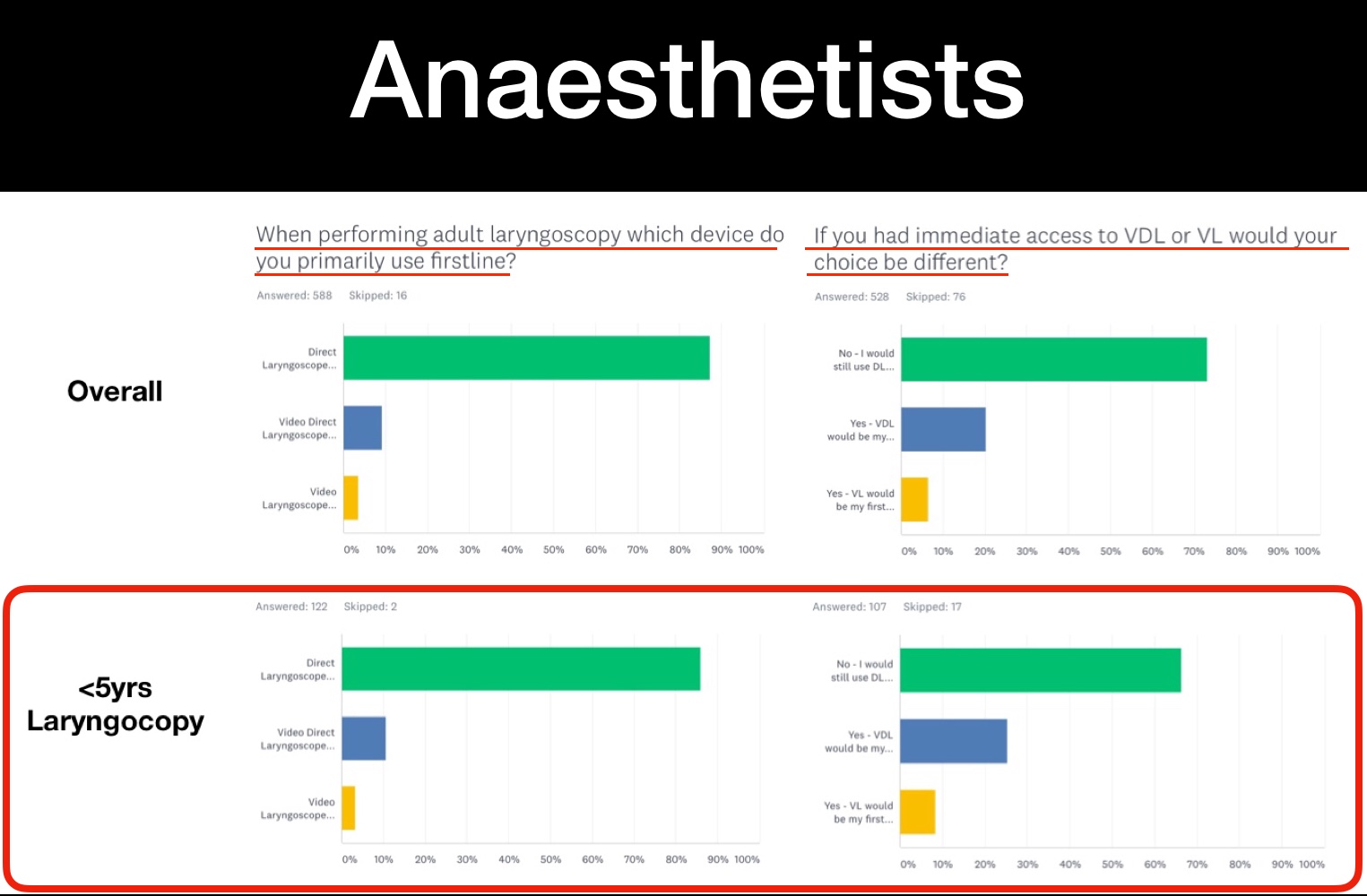
Within my own specialty, anaesthetics, trainees are frowned upon by the conformists for using video direct laryngoscopes – devices obviously better for patient care. They are made to feel inferior for not choosing first line to use a device designed in 1943 (the direct laryngoscope – DL).
So much so it becomes part of their psyche.
These attitudes and the attendant culture need to stop – instead healthcare staff must be nurtured to do what’s best for patients first and foremost.
However frameworks required to deliver ergonomic change will not simply happen with the passage of time – they’ll need to be forced in.
Within healthcare it is the highly influential conformists who resist ergonomic change the most.
It’s not that conformists won’t accept change – we have a constant stream of new drugs, medical devices etc entering healthcare – these innovations may appeal to the competitive nature of those in charge. Da Vinci robotic surgery has entered numerous public hospitals costing millions of dollars in taxpayers money despite 15yrs and over 4000 studies of evidence indicating no significant benefit to patient care.
Suggest innovations which make our work simpler, make it easier for us to succeed (ergonomic solutions) you’ll witness they’re often aggressively resisted.
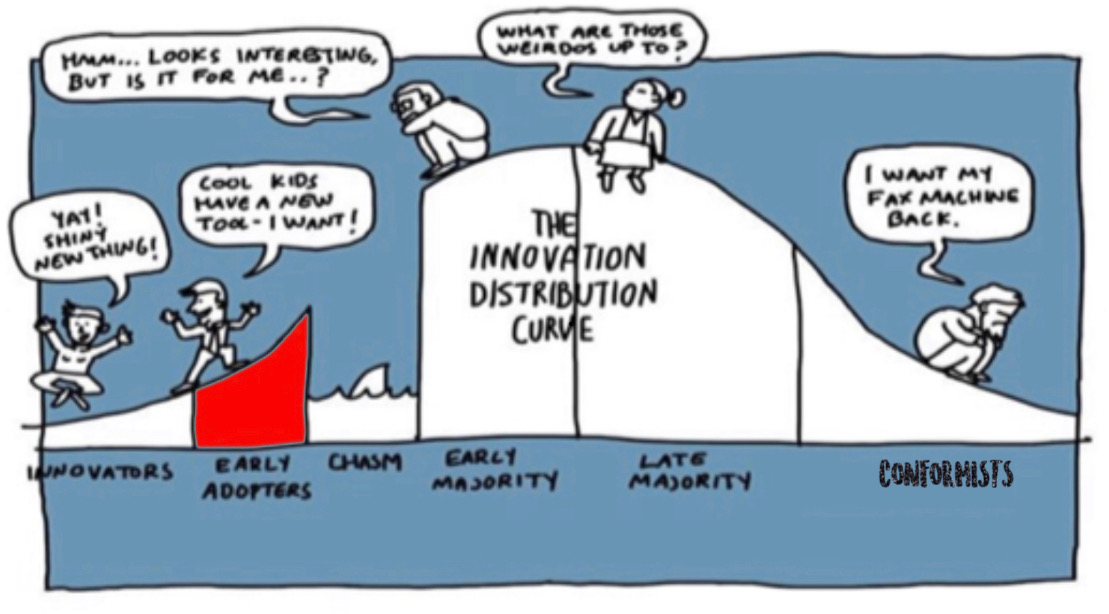
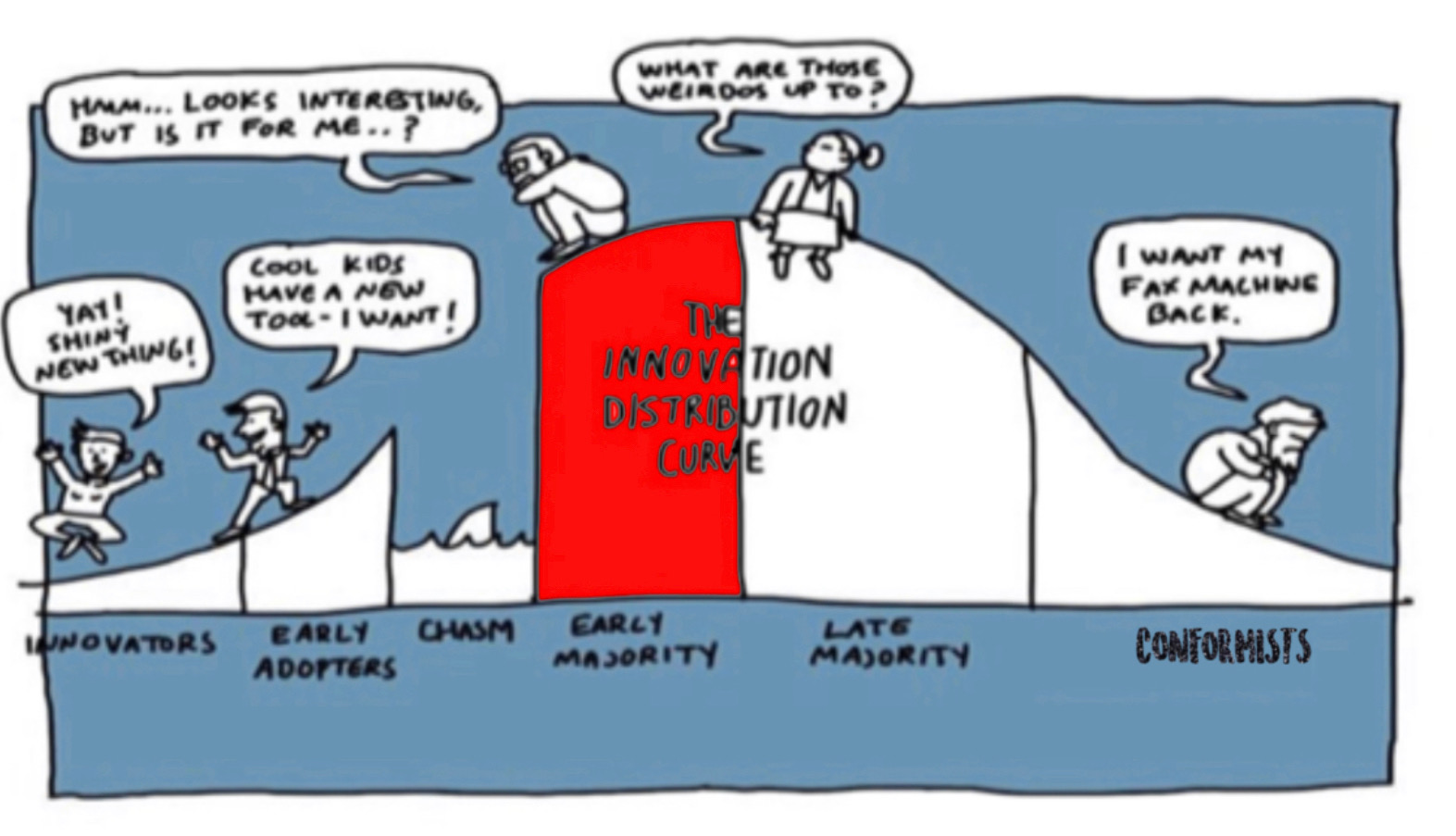
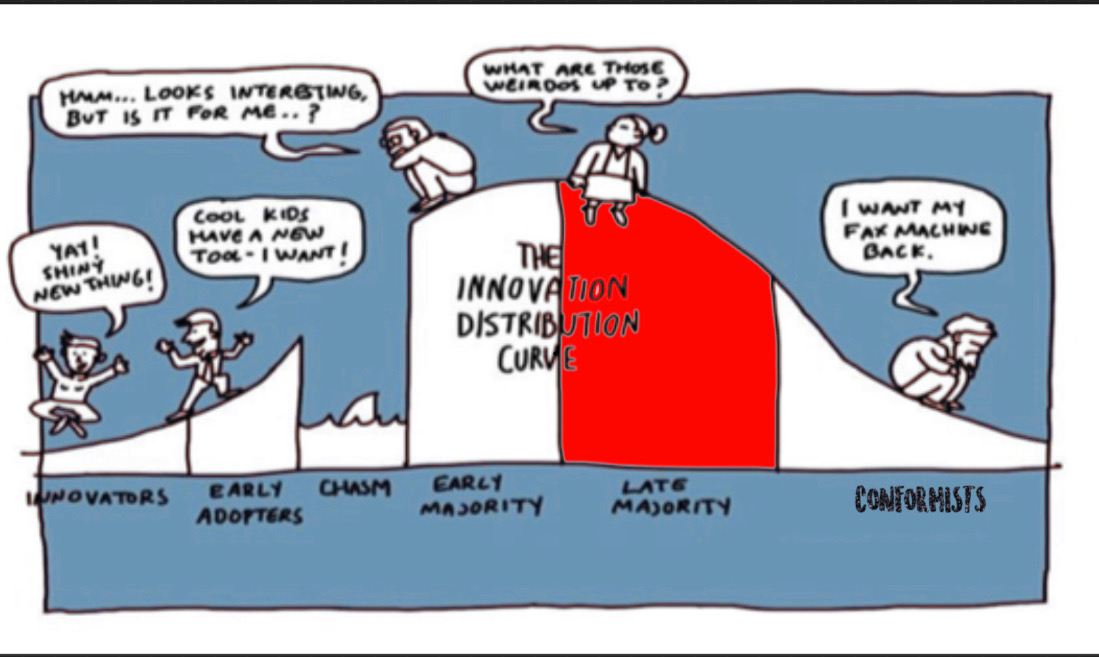
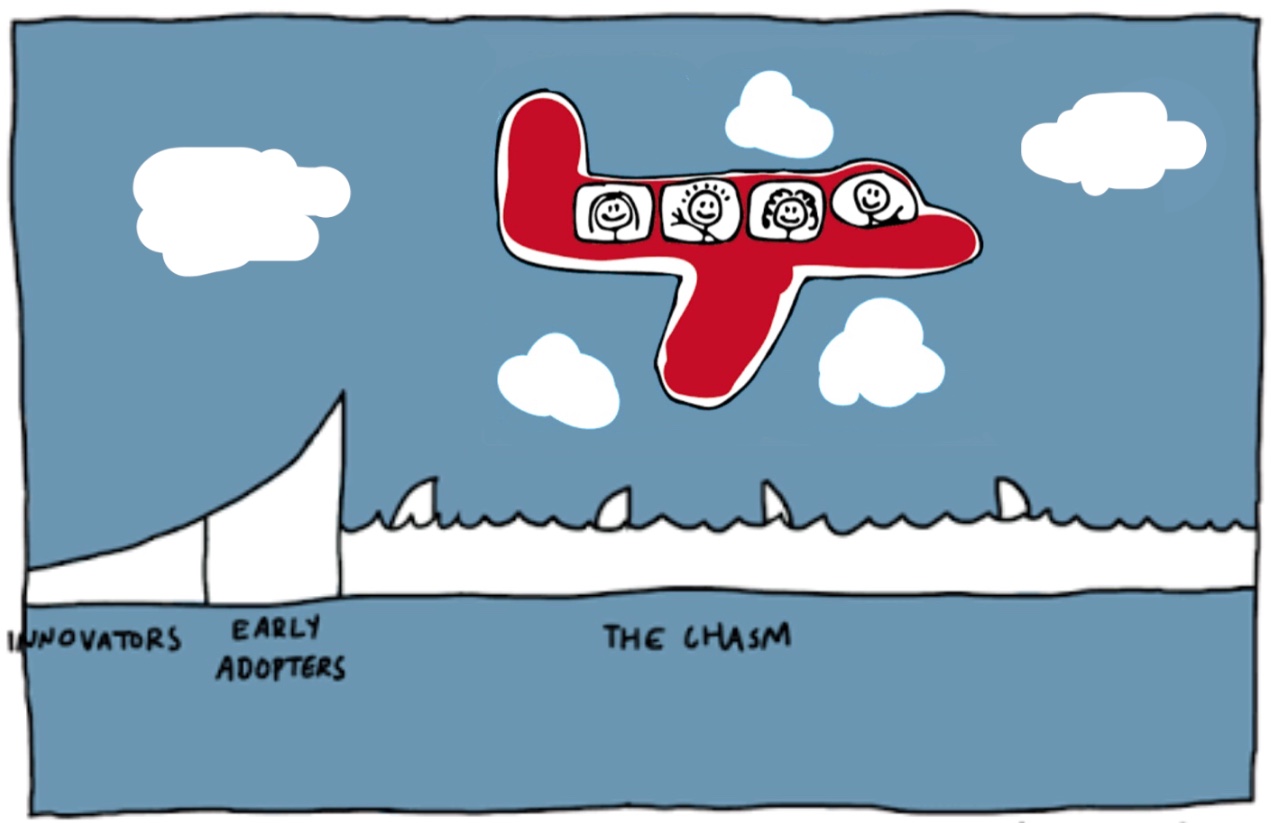
It’s perhaps easiest to explain how ergonomic changes are resisted through considering ‘Diffusion of Innovation’ Theory.
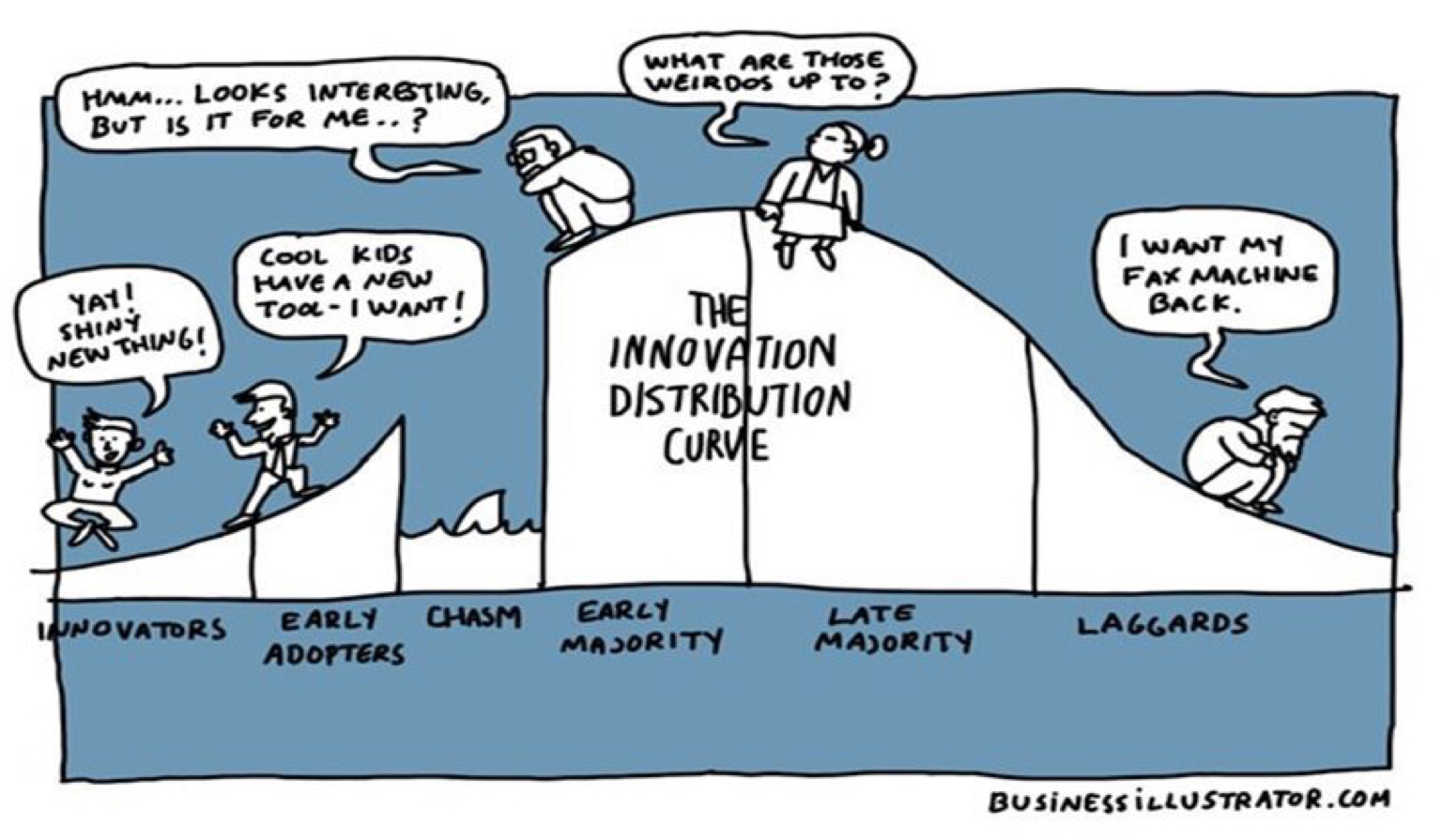
This model explains how new ideas, concepts, or practices can spread within a community. The introduction of ergonomic science can be seen as an innovation to be adopted across the whole of healthcare.
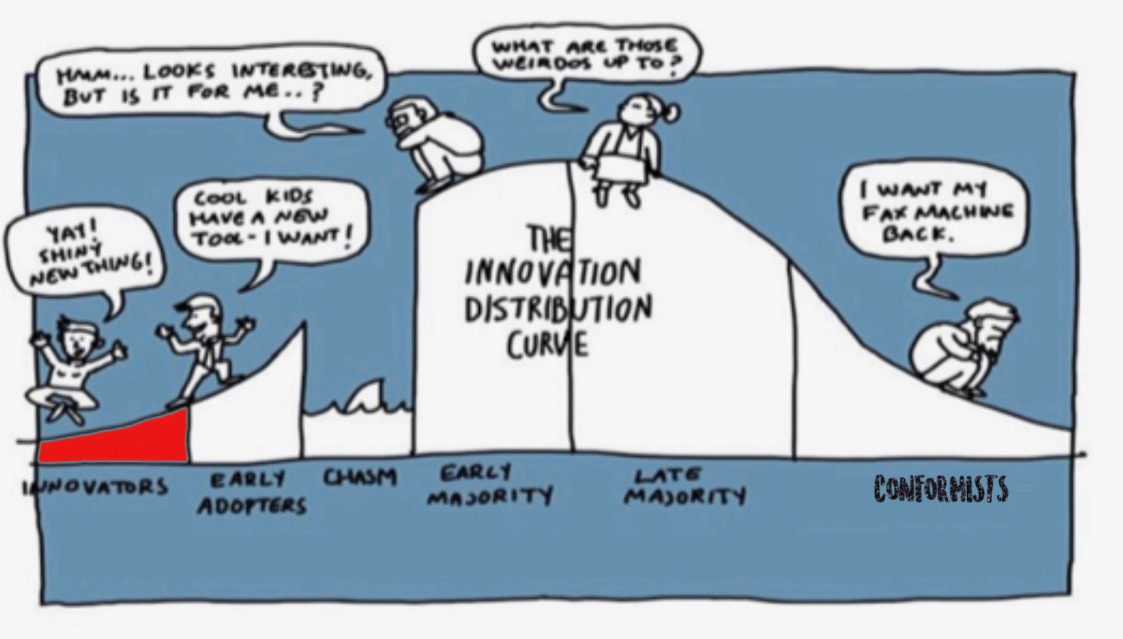
The pivotal step in diffusion of Innovation theory is crossing the chasm of change – it requires getting the early majority on board. However within current healthcare frameworks conformists may have too great a control over the early majority who fear their livelihoods should they step out of line.
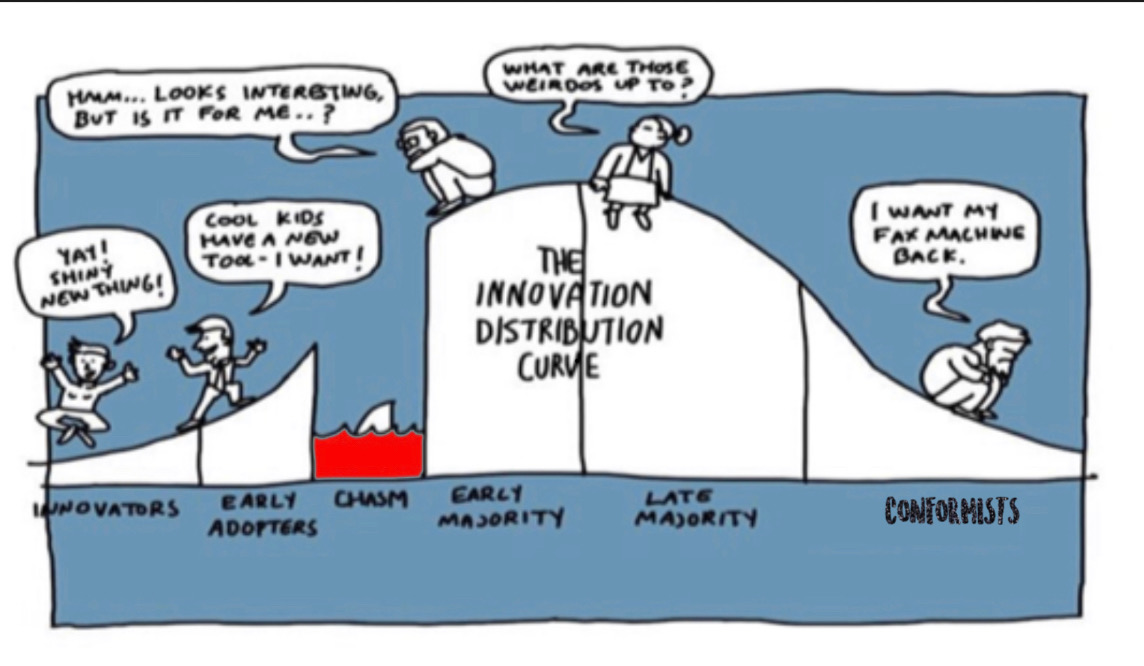
Perhaps for ergonomic science to cross the chasm will be impossible utilising indoctrinated frameworks of management – other ways of working will likely be required.
The #TheatreCapChallenge may symbolise one of tonnes of changes which need to be adopted for healthcare to improve. Perhaps in delivering frameworks which allow this initiative to become the norm we also deliver frameworks for many more positive changes to come – if we do succeed and we must – then we all win.
We’ll need to accept an uncomfortable reality – we haven’t always been doing what’s in our patients best interest – have the humility to bear this – to not is to perpetuate unnecessary harm.
For patient safety to improve we need a questioning culture – if we struggle this hard to adopt name and role theatre caps consider all the other initiatives which haven’t made it anywhere near this far.
If you work in operating theatres perhaps a simple way to gauge where you exist on the ‘Diffusion of Innovation’ graph is assess when you choose to wear a name & role cap with respect to the percentage of those around you doing the same.
Whatever your background, whether you work in healthcare or not and regardless of how extraneous you believe you are……..
Help.
Innovators (Whistleblowers)
Innovators: these are the enthusiasts in your organization. They likely hop on all innovations, and are willing to try anything out.
Perhaps in healthcare however they may eventually become the whistleblowers, ostracised from the industry thus removing much of their power to effect significant change.
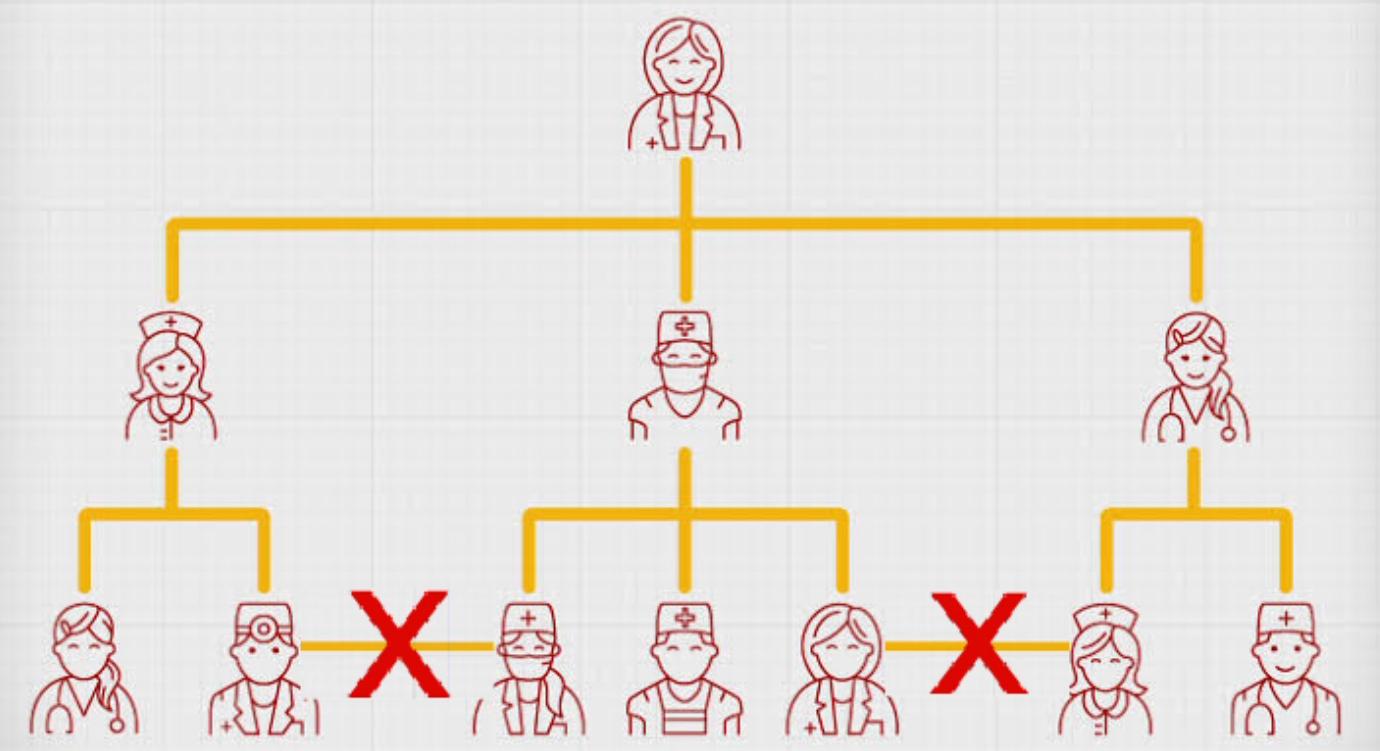
Healthcare like many other industries utilises top down structures for management. Those who work within the industry become conditioned to perform in accordance with this structure. Suggestions for change may be passed up to superiors .
Often a response from a superior to a change suggestion may be ‘no one else has complained about it’ implying there is an issue with the person suggesting change.
However some innovators persist despite this and the attendant risk to their own careers.
Why?
Perhaps they fear what happens if the industry doesn’t change more than they fear for their own careers.
Perhaps they fear adversity will only increase and patients and front line staff in turn increasingly suffer.
So they push on using whatever channels are presented to them – often speaking to others further up the chain of command. They may be encouraged too – yet without the support of others they may be exposed alone on the thin ice which cracks beneath them.
I have nothing but the utmost respect for Whistleblowers – they’ve often sacrificed so much for others – Dr Stephen Bolsin always springs to mind – one can only imagine the number of lives he’s saved yet as a result unable to find employment in the UK – exiled to the other side of the world. A part of the world where I work – yet believe me things on this side of the globe are no better – the Healthcare Safety issue is an international one.
Diffusion of Innovation Theory suggests instead of trying to convince conformists of the benefit of a change we should focus on gaining the support of the early adopters.
Sideways, lateral collaboration, however, doesn’t adhere to top down healthcare frameworks – one is not conforming with the norm.
You may be teased, harassed, threatened, intimidated, bullied for displaying your name and role on your theatre Cap.
However you can’t be sacked for doing something stipulated in healthcare policy – all healthcare staff must clearly display their name and role for others to see:
You’re doing the right thing – patients and society will thank you one day. So hold the line support is coming.
Early Adopters
Early Adopters: These are your best opinion leaders. Like the innovators, they are open to change, but they need to more clearly see the benefits before adopting a new behavior or idea.
As this infamous TED presentation from Derek Sivers explains the first followers are the true leaders.
Perhaps early adopters too understand if we don’t change patients will continue to suffer.
It’s vital the innovators look to obtain their support if the initiative is to succeed. The PatientSafe Network is set up to create collaboration between these passionate driven individuals much easier. The PatientSafe Groups allow great transparency so everyone can view projects being worked on and help drive them to fruition.
According to Diffusion of Innovation Theory it’s important that enough support is generated to convince the next group along to adopt the innovation.
Unfortunately the early majority sit on the other side of the chasm of change.
Early Majority
Early Majority: They are open to change, so long as you you clearly show them how and why it is good for your company. They will adopt after they have heard testimonials from the early adopters.
The early majority need to believe the initiative is safe to adopt. They are sympathetic to it yet need to know they’ll come to no harm. Self preservation is a key factor feeding into the bystander effect – one of the most replicable effects in social psychology.
Reaching this group is the hardest part of change management and involves crossing the chasm of change.
The early majority fear the impact on their own livelihood through doing something not dictated from above.

The conflict between doing what’s best for our patients versus what’s dictated from above can cause significant moral injury and psychological harm. Suicide rates amongst healthcare staff much greater than in the general population. Having come across a colleague who’d taken her own life perhaps it’s all too raw.
Humans (those in the majority groups in particular) are very strong social conformists. Further they’ll take comfort they’re supported from a legal standing given a significant majority of people are doing the same. This doesn’t however help deliver change and improvements in the care our patients receive.
The early majority may pity the innovators who become whistleblowers, perhaps feel guilty they didn’t do enough to support them, yet are glad not to be them.
They may internalise excuses that perhaps the innovators must have been doing the wrong thing. Perhaps they should have presented the initiative in a different way, used different techniques for communicating it – as if a ‘correct way’ exists to implement the initiative.
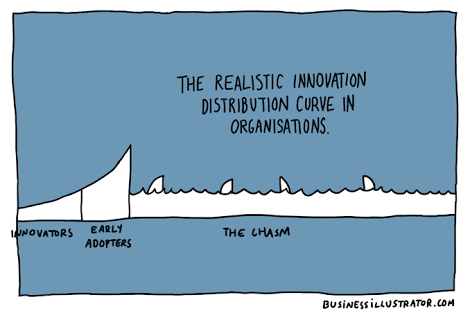
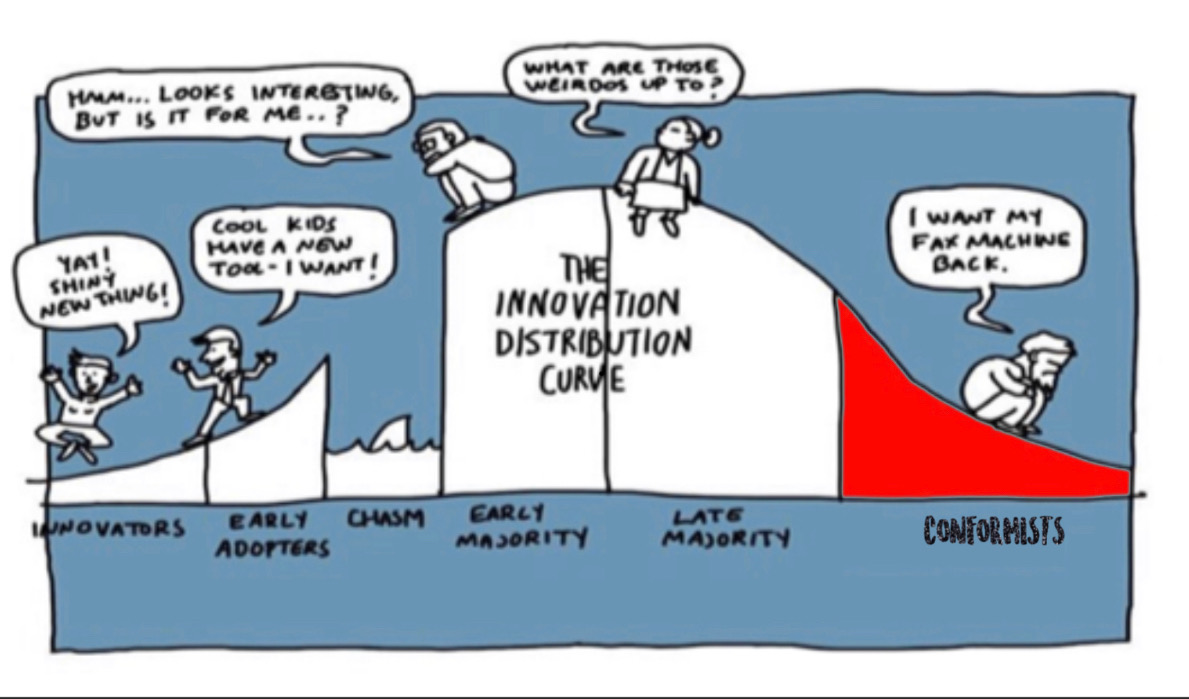
Perhaps however if there was a ‘correct way’ the initiative would already be the norm. Perhaps within existing healthcare frameworks there is no correct way to adopt these changes and the chasm for change in fact looks like this:
The early majority may say to themselves that the innovators should have known better than to step out of line.
This will be reinforced by others around them, particularly the late majority.
The Late Majority
Late Majority: This group is hesitant and not very keen on change. They will adopt change once they feel that they have to.
This group is very loyal to the institution. They fear the reputation of the institution being undone. Accepting we should have adopted a whole scientific discipline into healthcare may be too embarrassing for many.
One senior surgeon on social media described the #TheatreCapChallenge as ‘abhorrent’.
Doing the right thing for patient care – abhorrent?
We must be mindful of the impact these influential people have on the staff around them – how likely are the team he works with to be displaying their name and role?
Accepting change has at times been likened to bereavement – requiring the same emotional turmoil – denial, anger, bargaining, depression, acceptance. Who in their right mind would want to go through these emotions unless they had to? The late majority will be faced with constant reminders from the conformist group that they don’t need to – “things are just fine as they are”.
Numerous obstacles can be put up in the way – show me the evidence, cost, infection control. If the usual obstacles fail the late majority may be whipped into a mob and utilised as a force to isolate, ostracise, intimidate and attack the innovators.
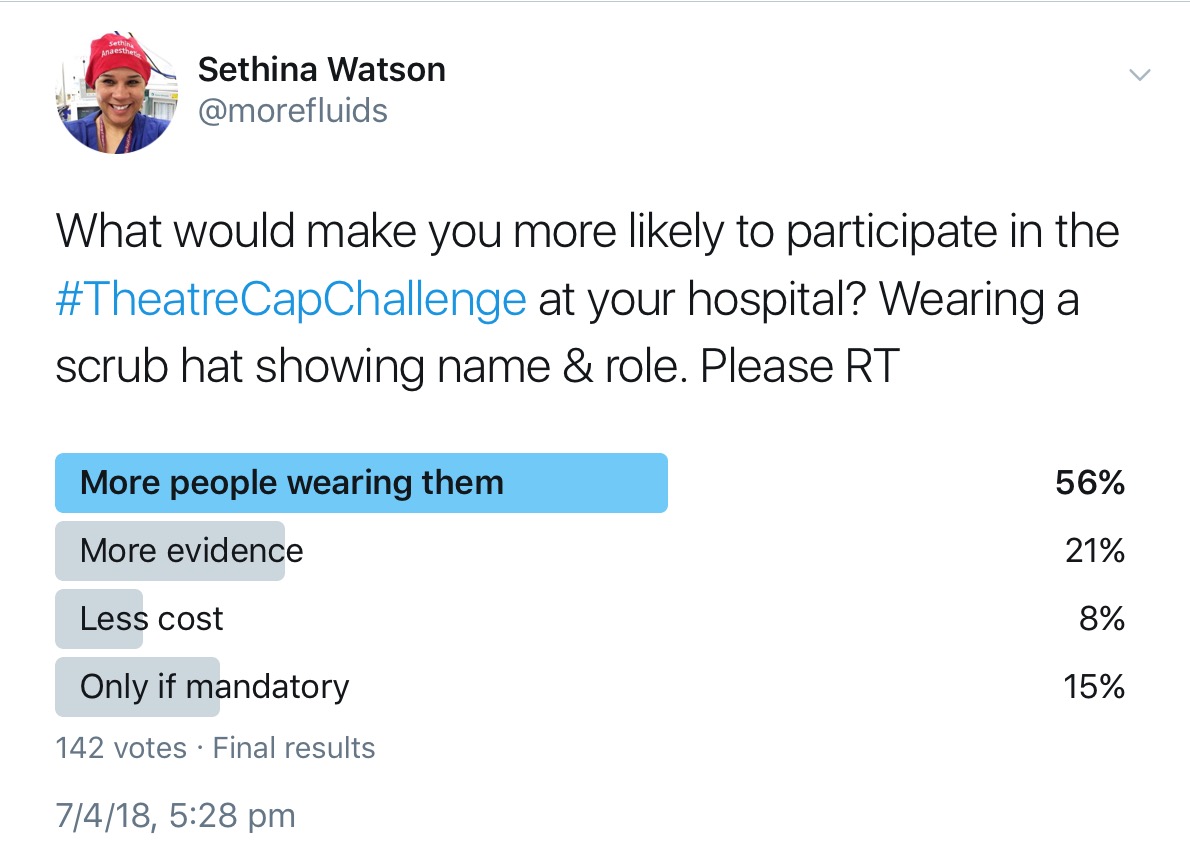
These comments from a nurse in the UK who was trying to organise a trial of name & role caps in her department:
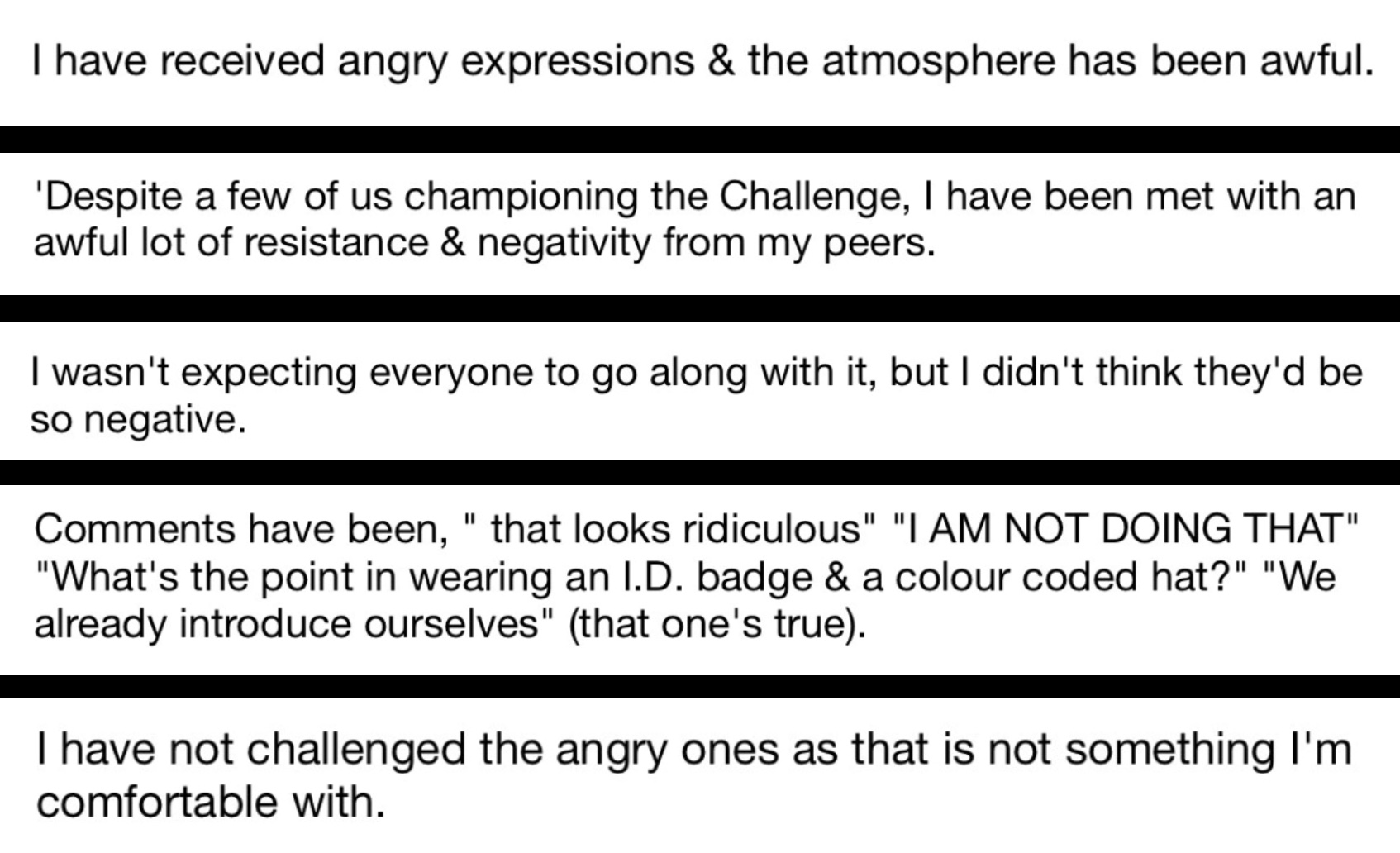
Social media can be a great platform to deliver this shaming.
I’ve put these images up to demonstrate some of the intimidation one may be subjected to – they’re from an anonymous account – having read about shaming I wouldn’t wish it upon anyone.
The late majority in supporting the shaming may believe they’re doing the right thing, preserving the integrity of the institution through attacking those who dare rock the boat.
Yet healthcare is an institution driven and maintained from generation to generation by the conformists.
The Conformists
Conformists: These are the very stubborn, reluctant-to-change authority figures. They will stick to their old methods and routines at all costs, and will only change their ways when there is no other option.
The conformists will go to every extreme to maintain the status quo – they’re emotionally invested in it – cognitive dissonance far too great.
The behaviour of these influential and often forceful few then going on to impact the whole culture of an institution
I’ve witnessed departmental heads resigning when their decisions are overturned only to have their decisions reinstated to keep them in their position.
As well as bullying, threats, intimidation I’ve witnessed departmental minutes being doctored and voted decisions being removed. At one institution we’ve been prevented for over 2 year simply from presenting the name and role cap initiative and recently I was threatened with legal action.
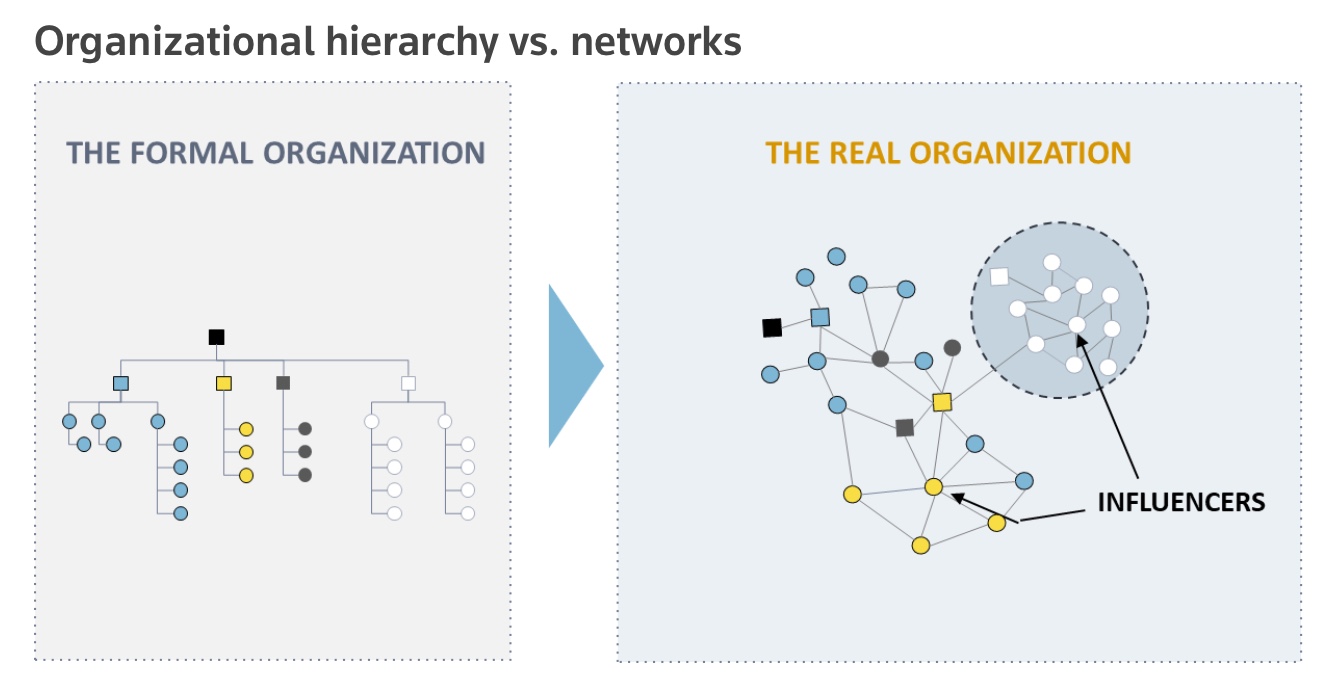
While the top down structure may appear a certain way on paper it often functions very differently.
Particular individuals able to exert significant influence on those around them. Even those above them on the hierarchical scheme often too fearful to challenge their behaviour for numerous reasons – respect, career aspirations, and to protect from the emotional trauma of change.
The status quo can be vehemently maintained at the expense of improved patient care.
So what is that drives conformists to these extremes?
What do they fear?
Loss of control? Losing their position of power?
Or is it something else much worse?
Is it shame?
Public shaming (putting people in the stocks etc) was ceased as a punishment in advanced cultures decades ago. It was seen by some as a fate worse than death. Reputations are destroyed, credibility lost. There is major psychological harm and risk of suicide.
We may falsely hope that when they retire they’ll be replaced by new people more accepting of change. Yet the top down structure rewards conformity – they’ll most likely be replaced by others most like them – conformists.
However if you believe that the conformists are the root cause of our problems and blame them for our issues then think again. You will find no solace – humans are humans – we do what we do when you put us in an environment. Understanding this is perhaps starting to understand ergonomics itself.
The conformists are just as passionate as everyone else in ensuring we get the best for patient care – they’ve just been conditioned to believe their way of doing things is the right way.
Finding someone to blame will not fix our problems.
We should be desperately sorry to patients, relatives and others we have harmed. We further compound their grieving through the lies and cover up used to used to maintain the reputation of an industry whose design is often utterly inept to help. The only avenue they often have left is to seek revenge and themselves find someone to blame.
Yet perhaps some harmed patients and relatives do approach contentment after the event. It seems to be those rare few gifted with a different path – one which helps them understand what is really going on – Martin Bromiley, Leilani Schwarzer – they work to fix the problems too.
For patient safety to improve we’ll need to understand ourselves and move beyond our conditioned and ‘normalised’ human tendencies.
If there is such a thing as a root cause then it is the healthcare frameworks themselves – introduce humans into them and this is what you get. Every system is perfectly designed to get the results it consistently achieves – in our case increasing adversity from medical error.
Since the late 1980s healthcare became overwhelmed with an astounding number of governance groups all utilising the system & frameworks outlined above.
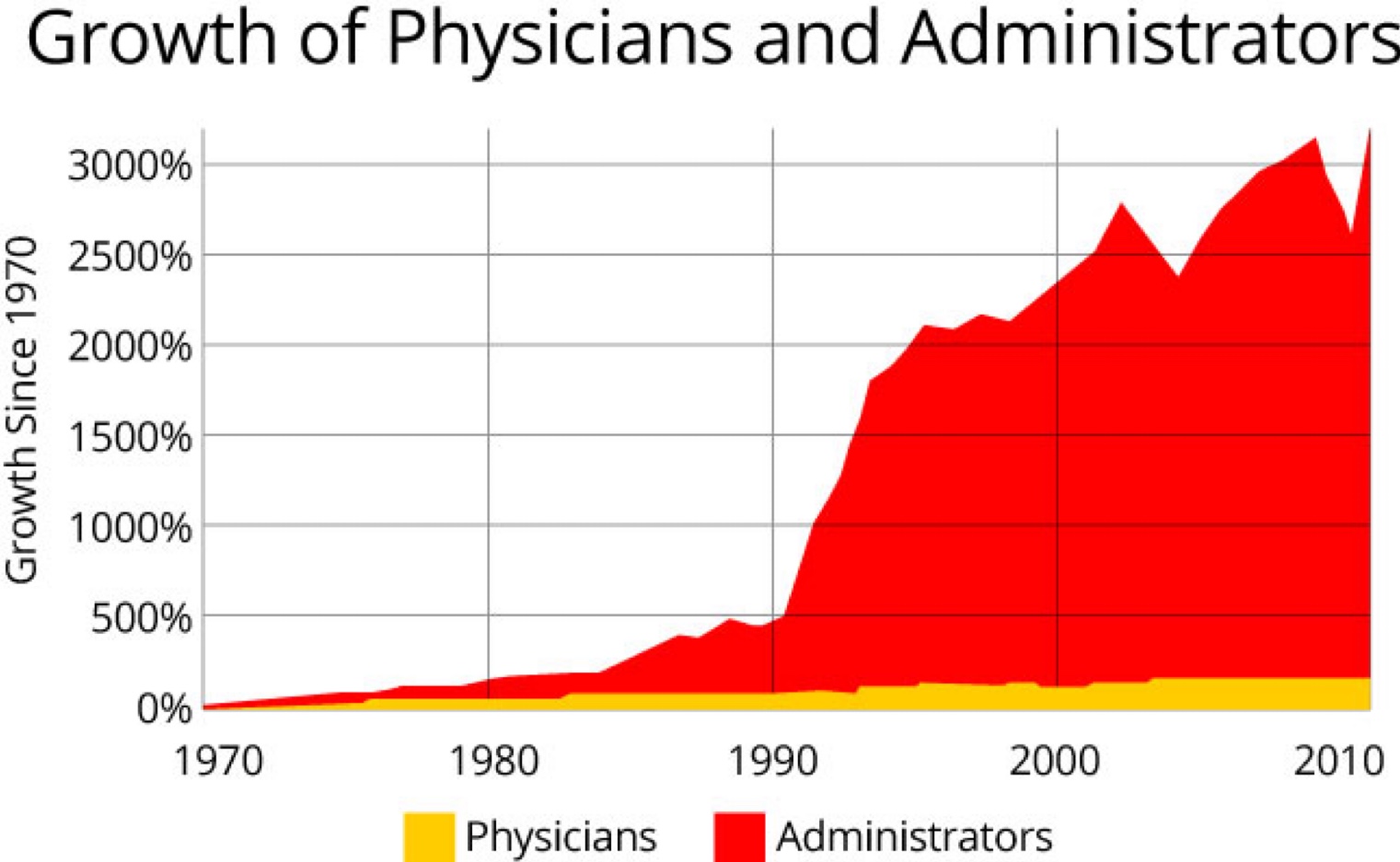
So much energy and expenditure wasted delivering nothing at best yet often worse – more complexity in the form of more policies, guidelines, education frameworks….
At the same time new drugs and equipment arrive on the front line – often untested. The FDA (US), TGA (Australia), MHRA (UK) despite being government agencies are all completely funded by the companies whose products they’re supposed to govern. Worse still the President of the FDA appears to have been put there by the companies themselves and when scientists within the FDA have complained about the safety of products their complaints have been dismissed and they’e been sacked. Through a loophole recently introduced 98% of the products that we interact with on patients do not require testing – they just need to appear similar to others that have already entered the market – it doesn’t matter if those other products have been recalled. If you find this hard to believe then watch ‘The Bleeding Edge‘.
Further the custodians of our error data keep it from us. Right now I’m still trying to obtain information I’ve seen indicating that ‘Electronic Health Records are the 4th greatest contributor to patient mortality in NSW’ – worse than sepsis. Clunky systems healthcare governing bodies have introduced harming patients in droves – and governing bodies are hiding this information away from the public eye.
With the increased complexity we become more likely to fail. Without sufficient safeguards in place our patients increasingly suffer. And on it goes……
Yes, it’s a very uncomfortable narrative but I’m not sure it can be sugar coated in any other way.
For those who defend the status quo this medicine may be too bitter to swallow yet it’s important we no longer allow them to stand in the way of change and improvement. While they do patients, relatives and front line staff are increasingly exposed to unnecessary harm.
They’re delaying what’s to come.
You see some ergonomic changes can get in.
How?
You may be lucky enough to work (or be looked after) in a hospital where the #TheatreCapChallenge has been adopted as the norm.
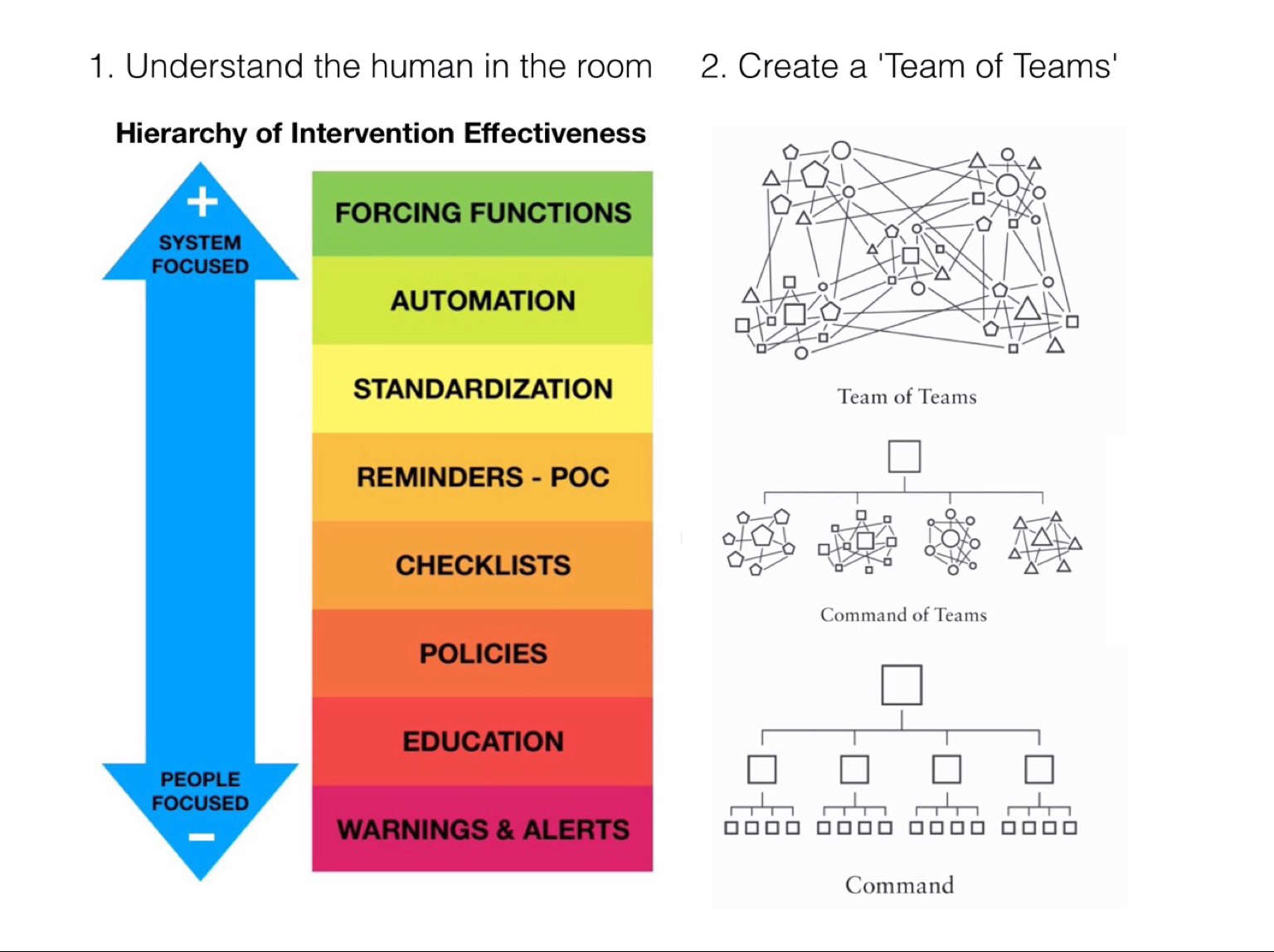
Consider how that came about and how the same frameworks which led to its introduction can be used to introduce numerous other initiatives. We need to understand the human in the room and work together openly as teams of teams with a defined goal – to provide the best environment for patient care.
Internationally numerous passionate individuals have worked together to continually deliver data to refine and support the #TheatreCapChallenge.
Thanks to the internet and social media we’re able to work differently now – rapidly collaborating and continually refining ideas always with the same focus – to deliver the best environment for patient care.
Innovators and early adopters coming together, demonstrating leadership in their own institutions to help initiatives take off.
Is the best way to get across the chasm to fly across it?
There are numerous patient safety and environmental projects underway across the world because of champions like you. The PatientSafe Network exists to provide you with all the support you need to bring them to fruition – everywhere. You can check out some of the projects here – get involved, join the conversations and look at all the information backing them up – you may have access to information and ideas others don’t.
When these projects reach a point where they’ll benefit our patients then safety champions everywhere can help drive them to fruition.
Check this one out for example ‘International Standardisation of the Hospital Emergency Number’. Unlike the external emergency number being fairly standardised across the world (911 US, 999 UK, 000 Australia) within Hospitals the Emergency Number varies wildly (eg Japan has 370 different numbers across 756 hospitals). There is an international drive to standardise the number at 2222 – you can help simply through finding out the numbers in hospitals near you – we will contact hospitals which haven’t standardised and provide them with all the information they need.
Be the leader you want to be – join the innovators and early adopters, collaborate and refine projects and make them as good as they can be.
Congratulate those champions who are doing the right thing, locate and support those who need help in getting there.
Perhaps the best way to create a path to improved patient safety is to show others where it is.
Let’s work together and create the best environment for patient care.