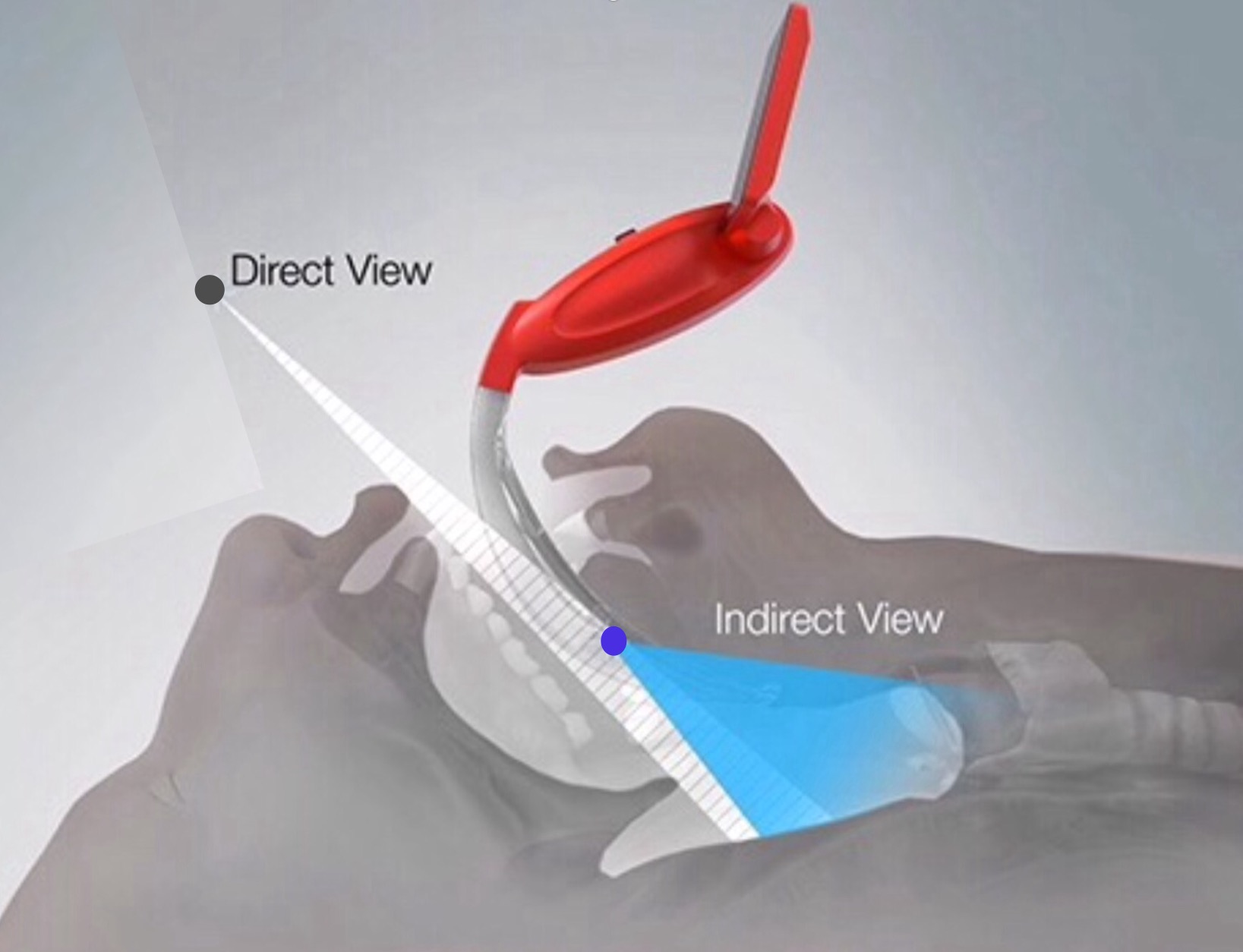
Devices allowing simultaneous video & direct laryngoscopy represent a safety advantage over either direct laryngoscopes or video laryngoscopes. Intubation is more likely to be successful, with less airway trauma (see here). Devices which allow a video laryngoscopic view for others to see are particularly helpful (see here).
In some centres the use of devices allowing video and direct laryngoscopy has already become the default technique for all laryngoscopic intubations in theatres and intensive care (see here).
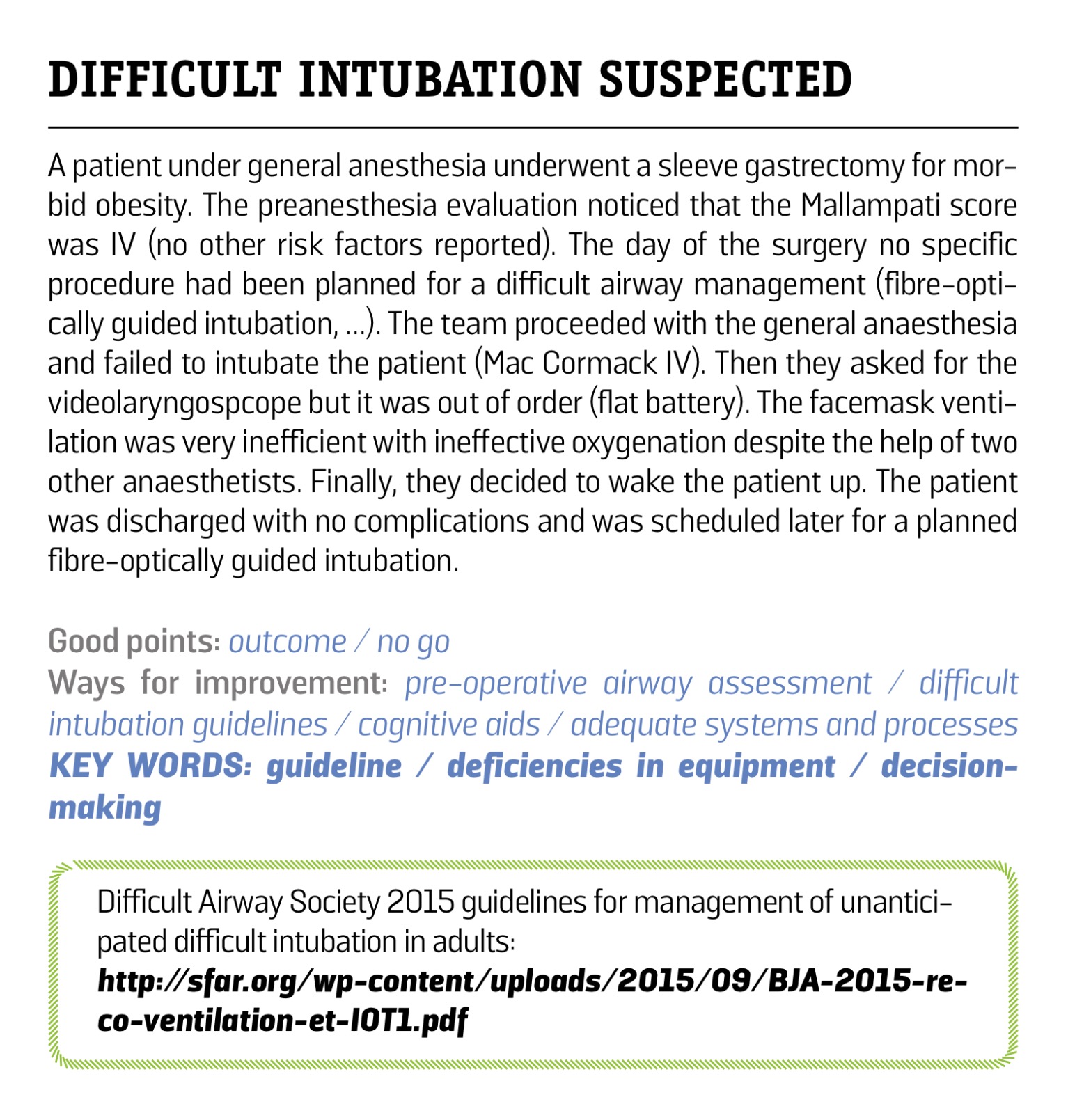
We often overestimate our ability to predict airway difficulty. In one study of 3991 difficult intubations 93% were unanticipated, and of 929 intubations predicted to be difficult only 25% were. (see here)
One retrospective analysis of emergency department intubations demonstrated an increasing number of adverse events with an increasing number of laryngoscopy attempts on a patient: adverse events 14.2% with 1 attempt at laryngoscopy, 47.2% with 2 attempts, 63.6% with 3 attempts, 70.6% with 4 or more attempts (see here). It would be prudent to ensure our first attempt is as optimal as it can be.
For those who feel trainees need to train with direct laryngoscopy otherwise they will become de-skilled this extensive assessments of over 14,000 intubations across 7 different centres appears Tom I spell that myth: The increasing prevalence of VL is not accompanied by a decrease in DL success.
The first attempt at intubation should be the best (and ideally the only) attempt. Laryngoscopes offering the combination of direct & video laryngoscopy serve this well. Optimal patient safety would allow all staff this choice, with video & direct laryngoscopes available to be used first line for adult patients.
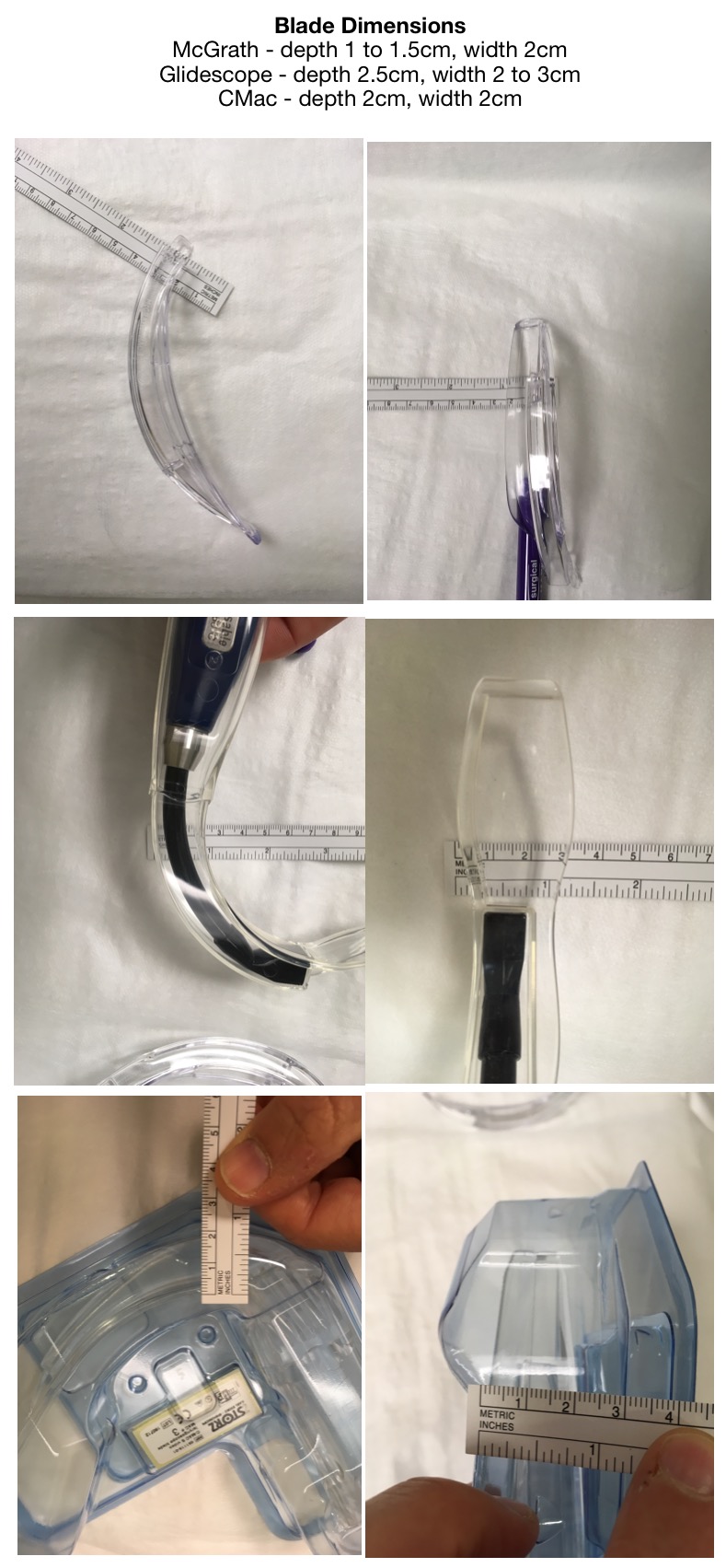
Not all video laryngoscopes are the same:
Those which allow video and direct laryngoscopy (VL&DL) simultaneously offer an advantage over those which are meant only for video laryngoscopy. (Soiled airway study)
Video & direct laryngoscopes which are smaller and easily portable provide an advantage over those that aren’t.
Channeled video laryngoscopes may disadvantage the user in only allowing intubation to occur in line with the channel. Non-channeled video laryngoscopes allow the freedom to manipulate the ETT – a patients anatomy may require this.
McGrath series 5 laryngoscopes may be temperamental – the screens occasionally blacking out because of poor contact between blade and handle.
Video laryngoscopes requiring a midline approach to laryngoscopy (such as the Glidescope) provide a less familiar approach to laryngoscopy.
Video laryngoscopes that allow the screen to be in front of you avoid you turning your head sideways during intubation.
Big screens and great optics improve the screen appearance however the bigger the screen the less portable the equipment.
The Airtraq is not a video laryngoscope, it is a dangerously inferior product that is detrimental to patient safety as some institutions may purchase it instead of a true videolaryngoscope.
When intubating with a VL&DL the assistant (and others) have a view. The assistant is able to visualise any necessary manipulation of the trachea, and will know (prior to any verbalisation) difficulties presented – in turn they can pre-empt next management step before you’ve even mentioned it.
The C Mac and McGrathMAC both offer VL&DL.
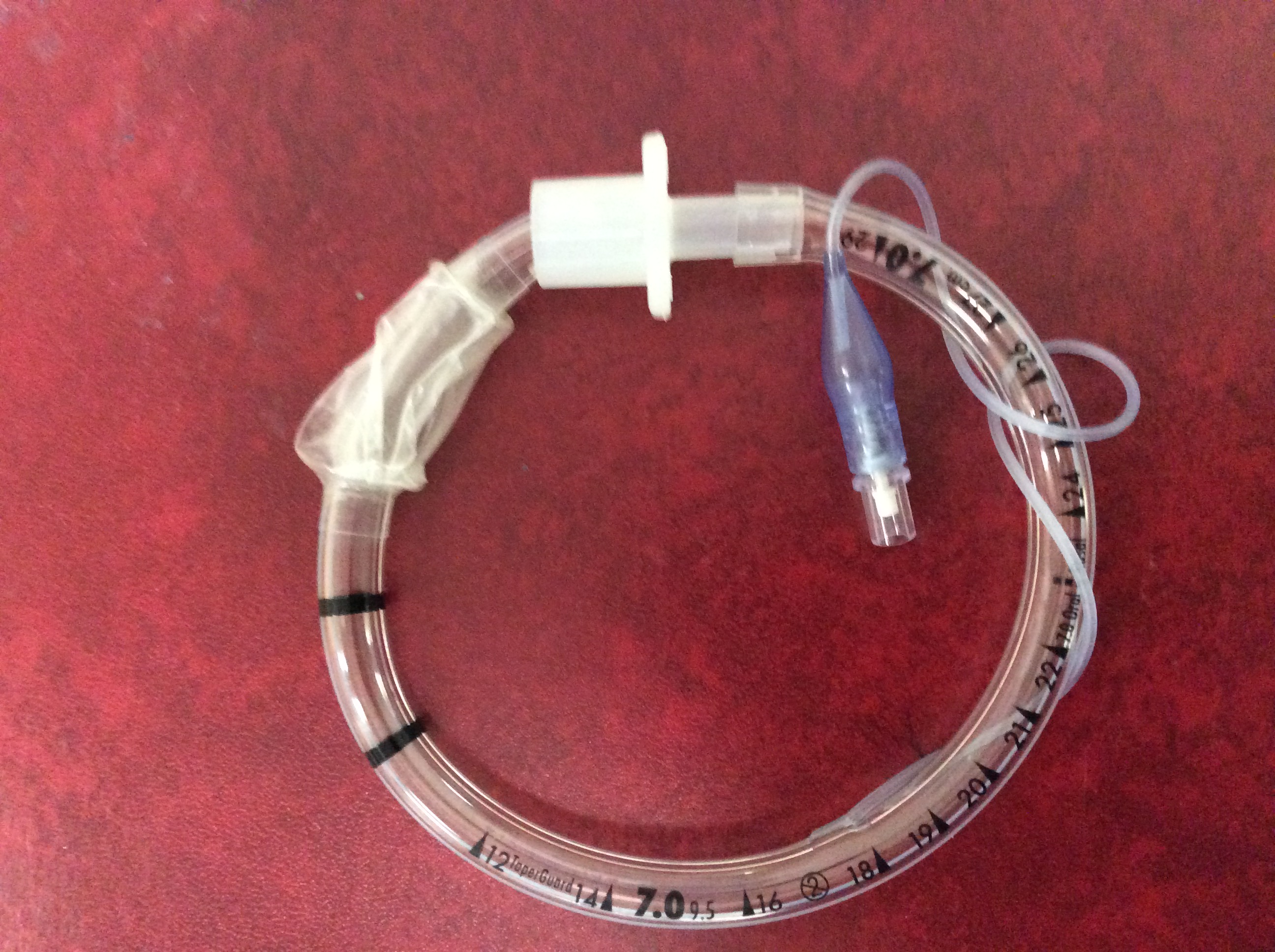
The blade on the standard McGrathMAC has a greater anterior curvature than the CMac. The CMac blade has the same curvature as a MacIntosh direct laryngoscope. It is important to be aware of this increased curvature – a stylet is more likely to be required with a McGrathMAC than with a CMac (see below).
The McGrathMAC has the advantage of being portable, and is positioned cost wise to allow numerous devices in multiple locations.
The disposable CMac blades & device have several ergonomic disadvantages compared to the reusable CMac device – the optics are generally worse and the blade dimensions are greater making insertion more difficult (see here).
‘Cost’ and ‘evidence’ are used inappropriately as tools to maintain the status quo. We discuss this further below. That video & direct laryngoscopes aren’t available already for all intubations perhaps reflects maintenance of the status quo by those higher in the chain of command – ‘this is the way we’ve always done it and we’ve never had a problem’.
Every system is perfectly designed to get the results it achieves. Currently medical error stands as the third greatest killer in hospitals – healthcare is perfectly designed to achieve this.
If we are to improve we need to accept change.
Some continue to support the routine use of direct laryngoscopes over combined direct & video laryngoscopes. We need to acknowledge the impact of cognitive dissonance and ego on thought processes which may detriment patient care. DL&VL laryngoscopes make honed yet imperfect skills in deciding when to use a video laryngoscope superfluous.
The MACMAN trial is often quoted to demonstrate no difference in first pass success at intubation with the McGrathMAC when compared with a direct laryngoscope. The authors note that the view obtained with the McGrathMAC is significantly better: grade 1 views achieved in 75.6% with McGrathcMAC vs 52.5% with direct laryngoscopy. However first pass success rate was quoted as the same in the 2 groups – the reason being but not quoted is that stylet use was prohibited.
Previous studies (see here) have demonstrated a stylet would be required in approximately 50% of occasions with a McGrathMAC and only 7% of occasions with a CMac or direct MacIntosh blade.
Stylets and bougies are recognised and oft used pieces of equipment for intubation – to prohibit their use profoundly impacts the results of this trial – first pass success rate with the McGrathMAC would have been significantly greater had a stylet been allowed.
The authors of the MACMAN trial should make the medical community well aware of this bias in their trial and consider repeating the MACMAN trial allowing use of a bougie or other methods of anterior curavture of the ETT.
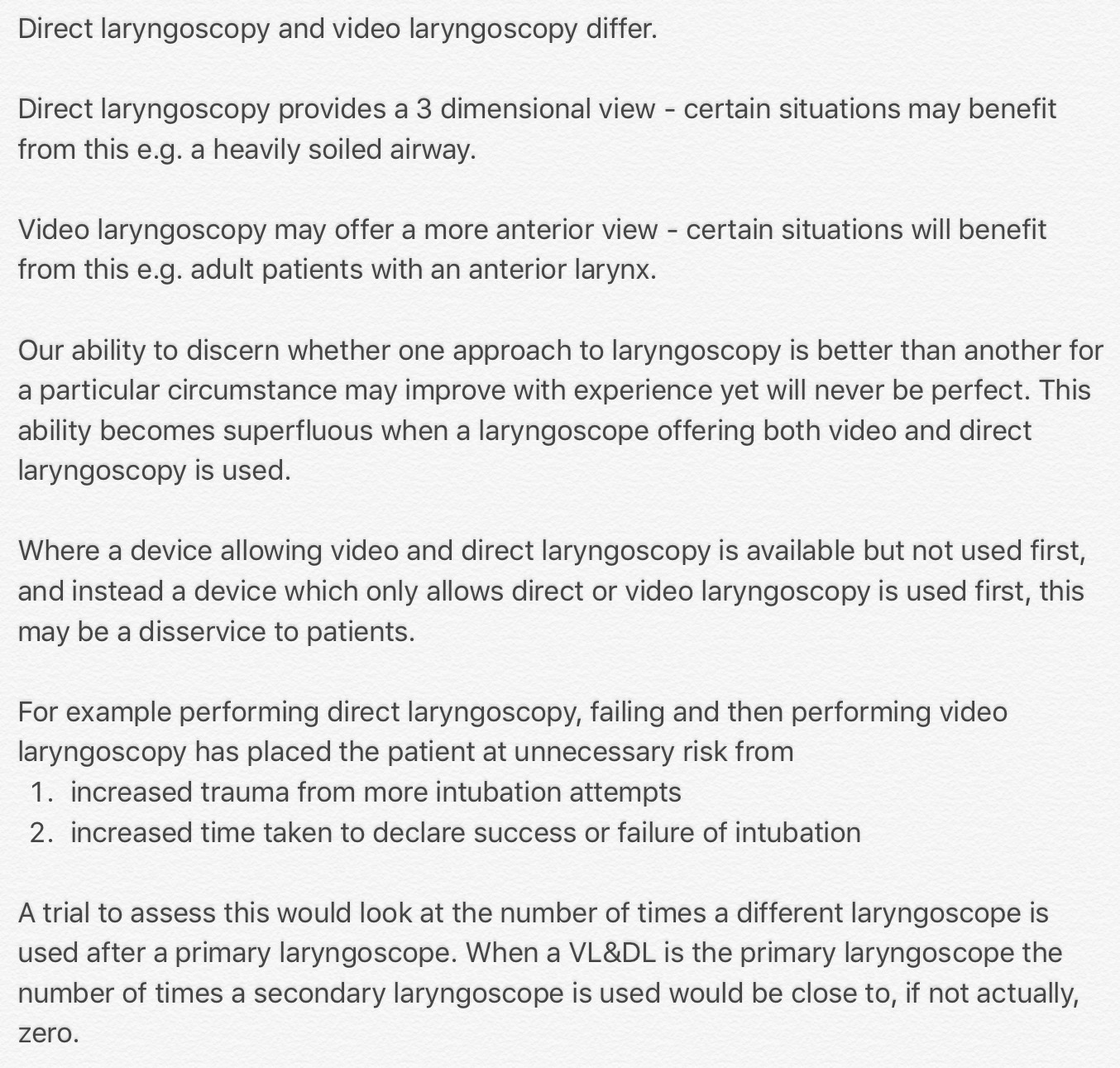
The image below shows the different curvature of endotracheal tubes and blades. From top to bottom
1. ETT with stylet in situ
2. ETT without stylet
3. Pre-circled ETT (see further image below and note how the curvature of this ETT replicates that of McGrathMAC blade beneath it)
4. McGrathMAC blade (note greater anterior curvature compared with MacIntosh blade)
5. MacIntosh direct laryngoscope
6. CMac direct laryngoscope (note curvature the same as with MacIntosh blade)

‘Circled’ ETT in image below maintains anterior curvature when released prior to intubation (number 3 in image above). This may avoid requirement for stylet when using McGrathMAC.
If one wants to use a VL&DL without requiring anterior curvature of the ETT then the evidence understandably favours using the C Mac (see here – this study demonstrates a 93% first pass success rate with a CMac vs 84% for direct laryngoscopy). (This study demonstrates 87.6 FPS for CMac vs 75.3% for direct laryngoscope)
A laryngoscope which offers both Video & Direct laryngoscopy will often be superior to either alone.
I work at an institution which may be unique in that all 26 theatres have their own McGrathMAC. Anaesthetists who work there, many including myself from an era before video laryngoscopes existed in theatre, accept that use of there is no benefit to the patient in using a direct laryngoscope instead of the McGrathMAC. A MacIntosh laryngoscope may occasionally be used for training in case one of us happens to work in an environment without a McGrathMAC, however many anaesthetists now have their own VL&DL device for use elsewhere.
Front end costs are often quoted as the limiting factor to the generalised introduction of VL&DL. In our institution there is a front end continuous cost saving after 400 intubations with the McGrathMAC – the McGrathMAC blades being $5 cheaper than the MacIntosh blades. Unfortunately, in healthcare our ability to quantify the financial loss of working without the best equipment is poor. As a result it’s difficult to assess the cost of failure to intubate well (with minimal sequelae) at the first attempt.
Until healthcare environments accept improvement change, it may be wise for those performing intubations at numerous different locations to purchase their own VL&DL, ensuring they provide their patients with the best possible care when it comes to laryngoscopy. Many critical care doctors have now taken this step.
Sadly the mark up on many VL&DLs is astronomical, to the detriment of patients and front line staff (see here).
Consider that those who may be faced with the most difficult intubations – paramedics – are least able to access the best tools – this needs to change.
Below we have listed what might be considered the best features of a laryngoscope. Please provide comment, feedback and any suggested revisions to this list
– most likely to be successful for most intubation scenarios
– VL&DL
– portable
– light weight
– robust
– low cost (laryngoscope handle, blades, batteries)
– decreased blade thickness for small mouth opening (see image below)
– NO blade channel
– blade angles: view using DL is as good as a Macintosh (C Mac provides this, McGrath has a curvier blade and you are much more likely to require a stylet or similar way of angulating your tube for intubation success)
– blade angles: ease of hyperacute (?attachment and access)
– optics
– still functions well in sun glare
– battery performance
– familiarity of use (use of laryngoscope replicates that of direct laryngoscopy – negates need to learn a different technique)
The cost of portable video & direct laryngoscopes will likely reduce as more brands enter the market place. Some are on sale for $500 US – perhaps you might obtain them for less.
There’s many more on this website (see here)
We provide a case report below where using direct laryngoscopy first line has ultimately lead to failure to intubate. The cost of this single episode in itself is likely to equate to the purchase price of 2 VL&DL even at their inflated price.
It’s time we started putting our patients care ahead of our ego:
PatientSafe has no financial interest with McGrath, Covidien, or any other suppliers of this product.
We welcome the introduction of similar products to the McGrathMAC – their introduction to the marketplace will competitively improve the price.

2 Comments