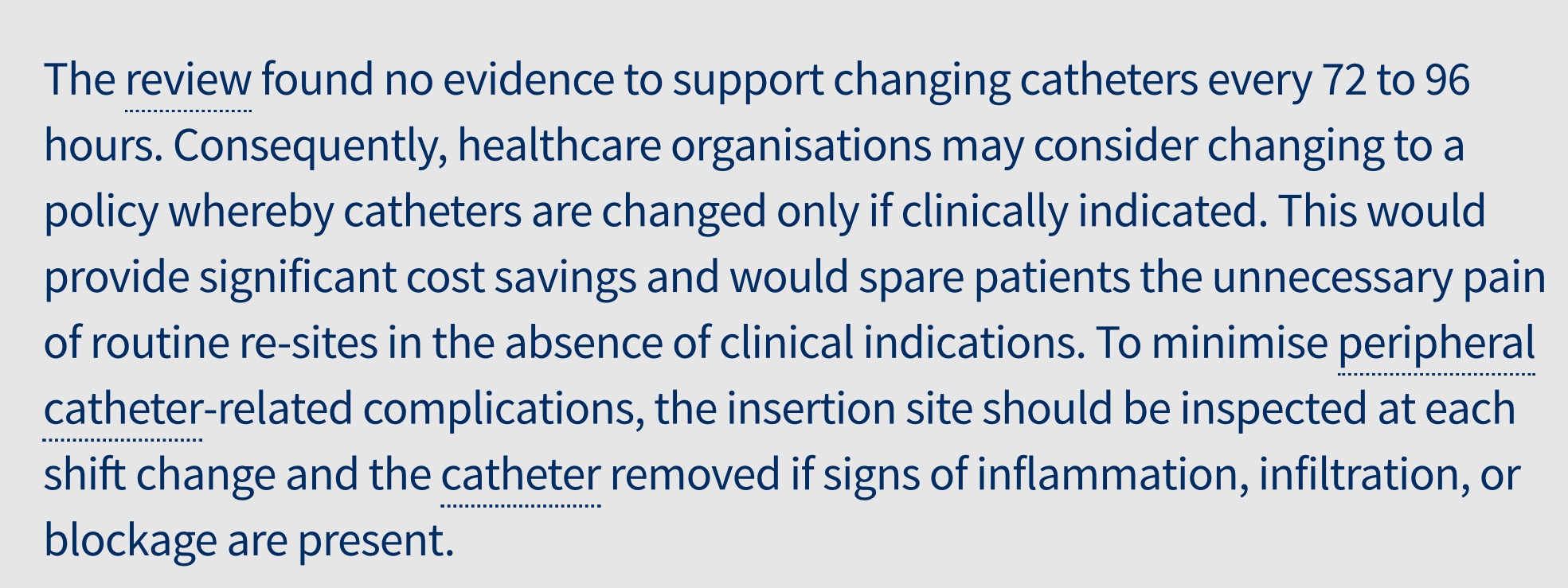
 A Cochrane review published in August 2015 (see here) found no evidence to support the routine changing of peripheral intravenous cannulae every 3 to 4 days.
A Cochrane review published in August 2015 (see here) found no evidence to support the routine changing of peripheral intravenous cannulae every 3 to 4 days.
Healthcare facilities should consider a policy whereby catheters are changed only if clinically indicated.
The implications of this for reducing unnecessary workload on the front line are great.
Help:
If you know of any institution which has a policy of routine replacement of peripheral cannulae then please forward this Cochrane review to the hospital managers.
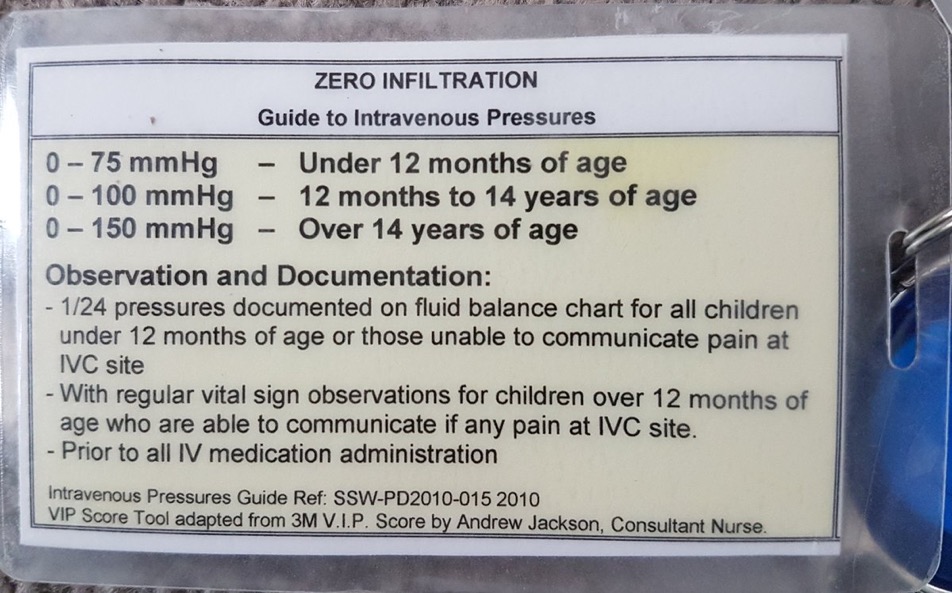
The AVATAR group have provided some excellent resources outlining how best to assess peripheral venous cannula sites (see here).
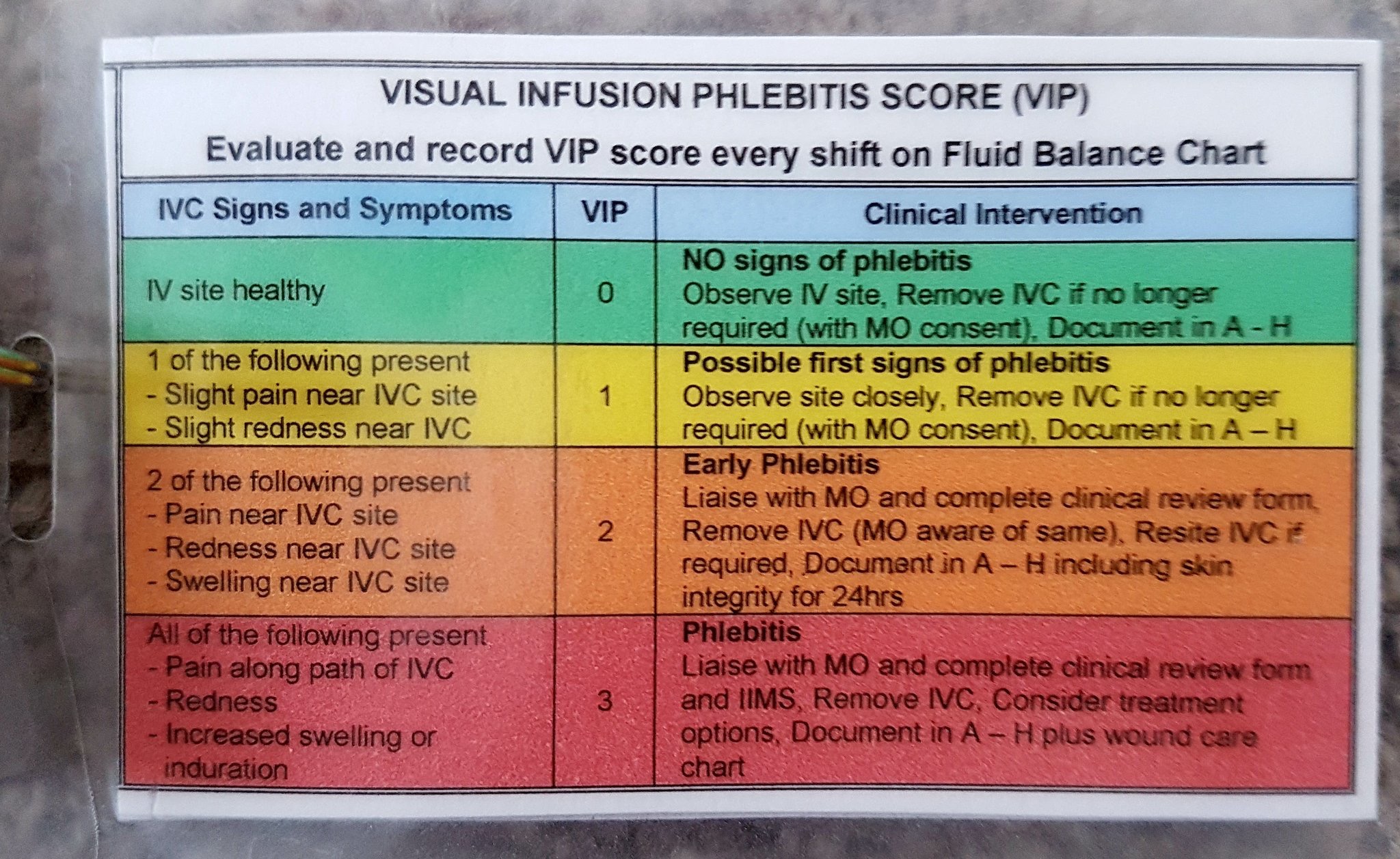
The VIP (Visual Infusion Phlebitis) score provides a way to assess peripheral cannula sites:
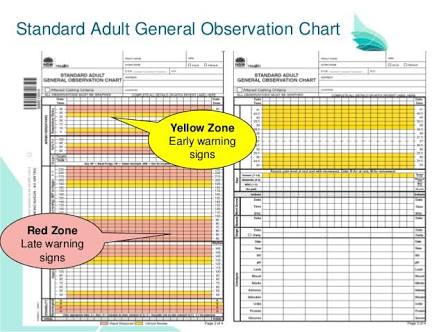
Perhaps a convenient place to assess cannula insertion site every shift would be on the patient observation chart. We highly recommend hospital managers review the benefits of the ‘Between the Flags’ system of patient observation charts developed in NSW, Australia (see here).
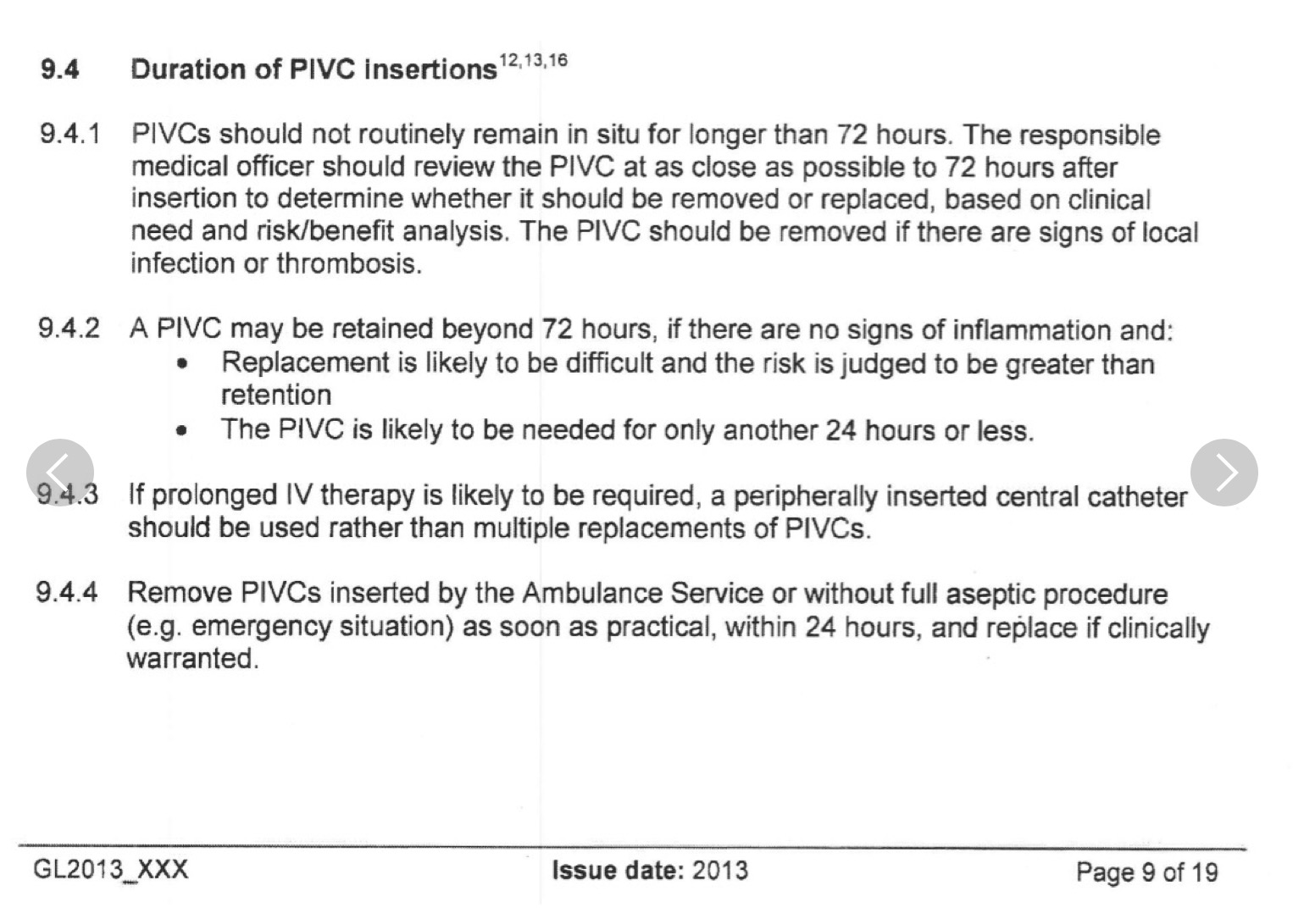
Below is the relevant section of the current NSW policy concerning the management of peripheral intravenous cannulae – we would like to see this changed (click here for full policy):
You may want to contact NSW Health to update this policy so that it is consistent with the best available evidence.
You can send them an email via this link: http://www.cec.health.nsw.gov.au/get-involved/contact-us
It is also worthwhile noting that the regular unnecessary replacement of peripheral cannulae may increase a patients risk of having ‘longer term’ venous access requested. These longer term intravenous access devices have a very high complication rate:
– PICC lines – 1 in 4 have major complication (see here)
– Central Lines – have a high complication rate, for example at least one patient dies every day from an avoidable central line air embolus (see here)
In the UK the STOP campaign is being used to make clinical staff think twice before inserting any invasive line into a patient and assessing if they truly need it given the potential risks (see here).

11 Comments