
‘When faced with a human error problem you may be tempted to ask ‘Why didn’t they watch out better? How could they not have noticed?’ You think you can solve your human error problem by telling people to be more careful, by reprimanding the miscreants, by issuing a new rule or procedure. They are all expressions of the ‘Bad Apple Theory’ where you believe your system is basically safe if it were not for those few unreliable people in it. This old view of human error is increasingly outdated and will lead you nowhere.’ – Sidney Dekker.
Current health care safety lends upon ‘Bad Apple Theory’ relying on alerts, education and policies in response to adverse events.
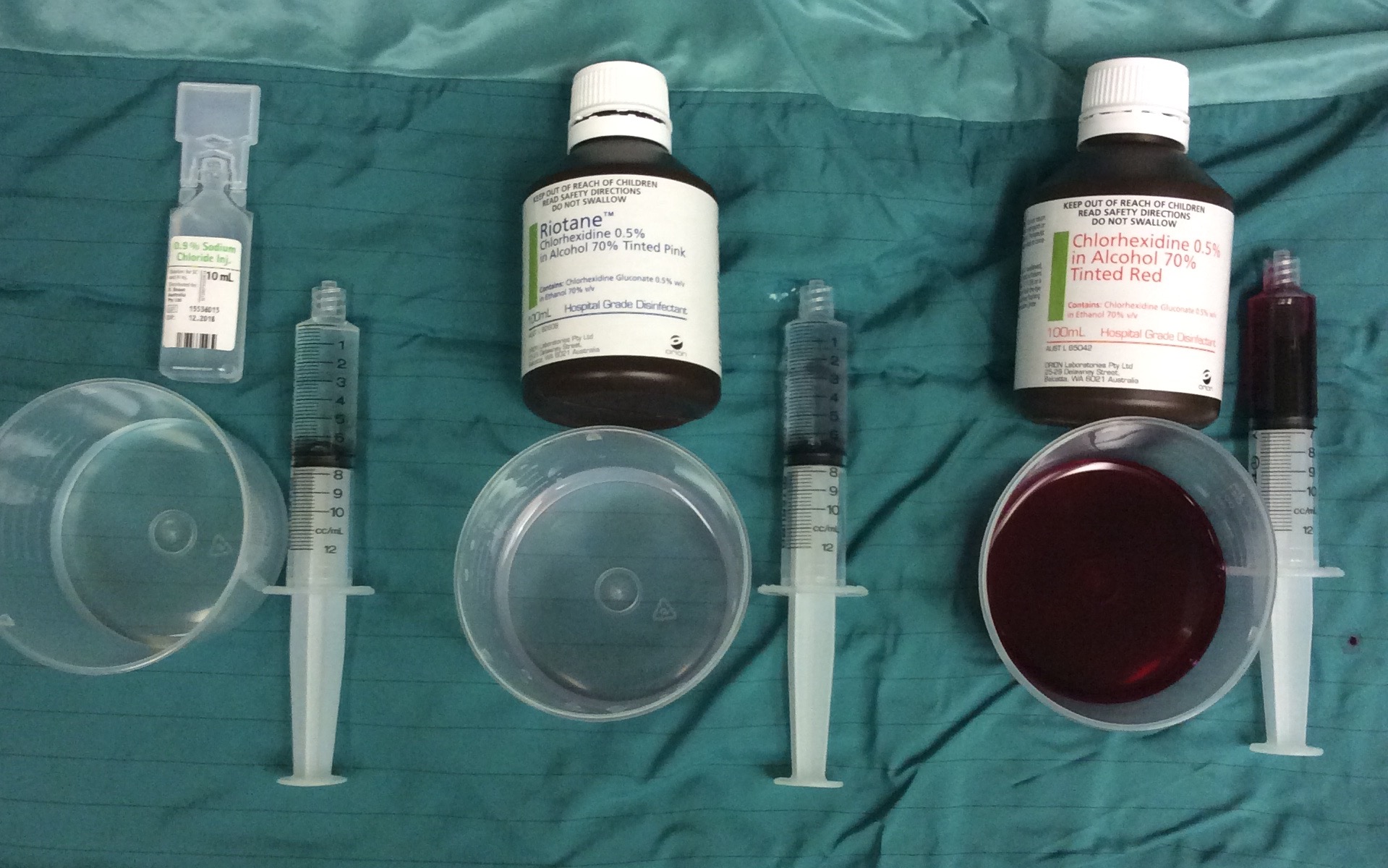
In 2010 Grace Wang was paralysed when indistinct chlorhexidine (solution centre of image) was mistaken for saline (left of image) and injected into her epidural. Distinct chlorhexidine (right of image) and non-pourable versions are used without problem and at no extra cost in many institutions.
Grace is one of hundreds of patients who’ve suffered because this unnecessary hazard exists in our hospitals (see here).
The NSW Health response to the Grace Wang incident was an alert outlining essential procedure when using antiseptic solutions:
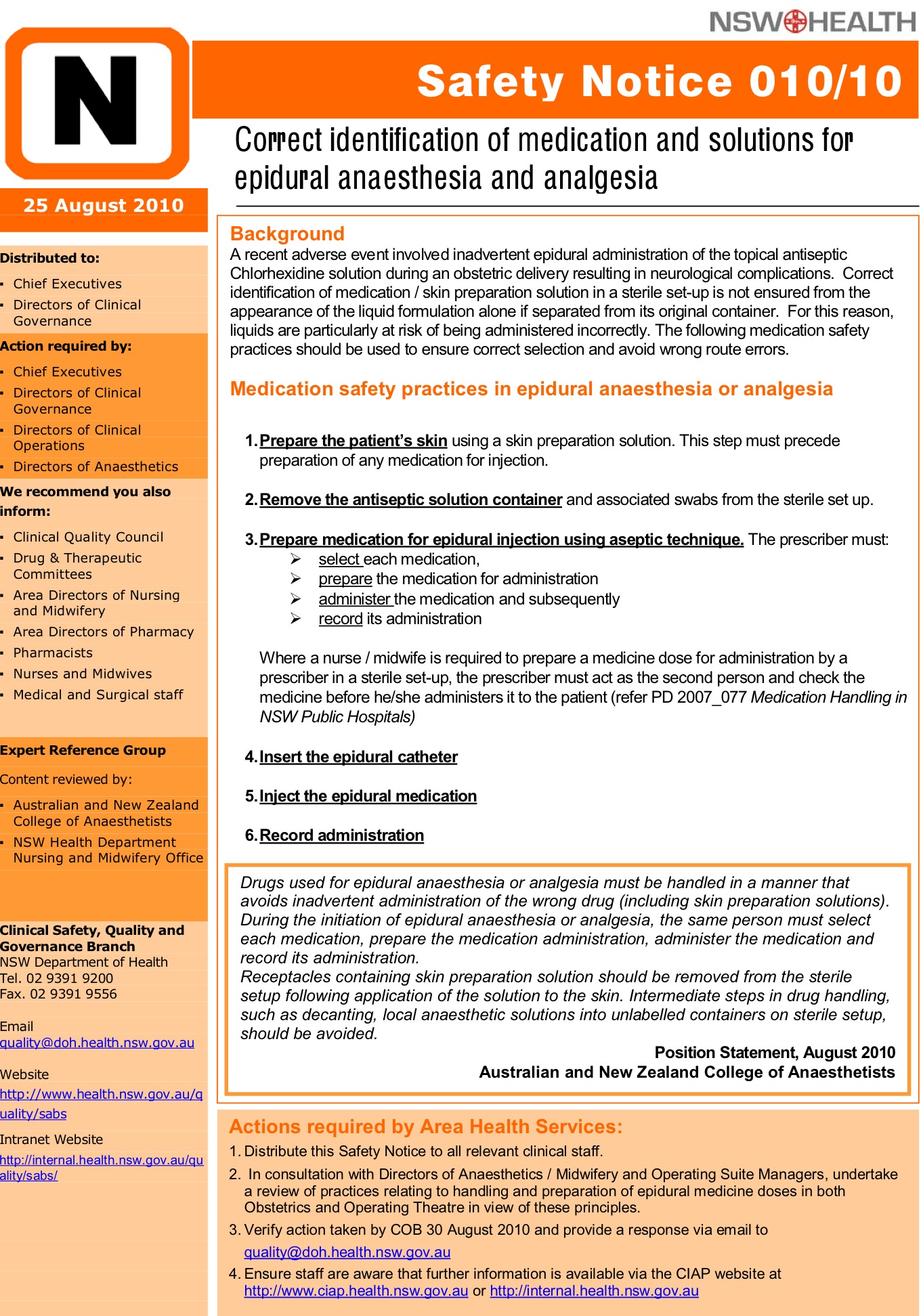
Alerts such as these are part of the top down safety response which is used in healthcare. Many years ago an alert like this may have had some effect, however healthcare is now too complex for interventions like this to have sufficient impact.
Human Factors Engineering teaches us this alert has not created a safe system leaving patients at unnecessary risk.
The Root Cause Analysis performed after the St George event (see here) recommended antiseptic solutions be distinctly coloured – this recommendation has not been instituted.
There have been no reports of mistaken administration when distinct or non-pourable chlorhexidine is used. Front line staff do not want indistinct pourable chlorhexidine in hospitals. Over 600 people now have signed the petition requesting it be banned. We understand the complexity of our work environments, that slips and lapses occur and ‘to err is human’. We fear for our patients and fear for ourselves becoming the next ‘second victim‘.
Given that banning indistinct chlorhexidine appears a simple safety solution, why hasn’t this already been done?
Perhaps legal ramifications and the repercussion from manufacturers makes regulating bodies (TGA, FDA, MHRA etc) hesitant to act.
How do we instill courage in governing bodies to provide us with safer work environments?
When indistinct chlorhexidine is banned know that this has happened (please sign the petition here). We will have gifted ourselves with a framework to start optimising patient safety.

3 Comments